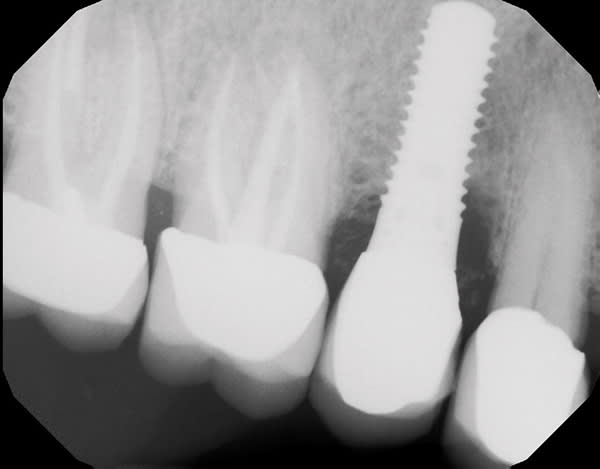
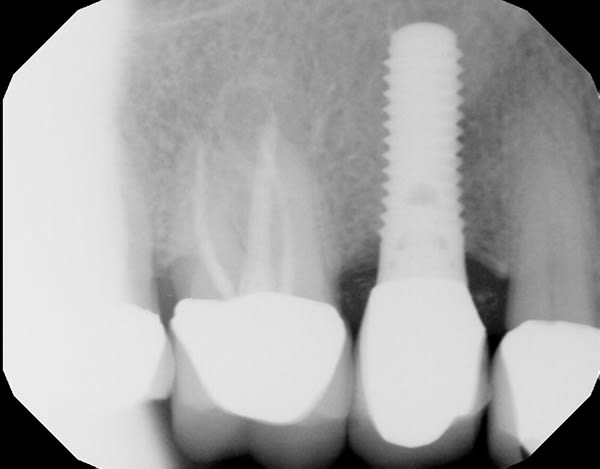
A 63-year-old male patient was referred in 2015 after a routine cleaning at his restorative dentist revealed pocketing and heavy bleeding on probing (BOP) around an implant in site No. 4. The implant (Straumann RN TE) had been placed in 2003 under the author's care due to a previous root fracture of the endodontically treated tooth No. 4, which had been extracted 6 months prior to presentation. The final implant crown was cemented with a polycarboxylate cement in 2003. The patient was highly compliant under his general dentist's care with regular 6-month prophylaxes. In 2015, the patient presented as a healthy non-smoker with a controlled medical history of atrial fibrillation and high cholesterol. Parafunctional habits were contributory to the failed tooth. The patient was diagnosed with site-specific beginning-to-moderate peri-implantitis around No. 4. LAPIP treatment using the PerioLase® MVP-7™ Nd:YAG laser (Millennium Dental Technologies, lanap.com) was performed. At 2 weeks' follow-up, the patient reported 0 out of 10 on a discomfort scale. He maintained good plaque control and returned to his restorative dentist's care after 6 months of healing for alternating periodontal maintenance visits every 3 months. At 7 years' postoperative, the peri-implant tissues associated with No. 4 were healthy with ≤4 mm probing depths and light BOP.
KEY TAKEAWAYS
The free-running pulsed Nd:YAG laser-based LAPIP protocol (laser-assisted peri-implantitis protocol) enables effective treatment for peri-implantitis in a single visit.*
The minimally invasive LAPIP protocol reduces the bacterial load and thus controls the localized infection.
LAPIP therapy elicits minimal postoperative discomfort, minimizes postoperative recession, and is preferred over conventional treatment by patients. Return to gingival health and significant bone fill are typical long-term outcomes. This case included post-treatment visits every 2 to 3 weeks for prophylaxes with a hygienist and review of plaque control measures until 3 months post-procedure, followed by a 3-month periodontal maintenance protocol.
*See author's note at the end of the case presentation regarding cases with resin cements.
Robert A. Levine, DDS
Private Practice (ret.), Philadelphia, Pennsylvania; Diplomate, American Board of Periodontology; Fellow, International Society of Periodontal Plastic Surgeons; Fellow, Diplomate, Academy of Osseointegration; Fellow, International Team for Implantology