Abstract: Often times patients present with an immediate concern, however other underlying problems may exist that might also need to be addressed in order to fully resolve the issue. In this case report, a patient presented for a limited examination and immediate treatment of a fractured mandibular right molar. She also had concerns regarding tooth wear, other fractures, and esthetics. Her high smile line revealed uneven gingival margins and a “black triangle” between teeth Nos. 9 and 10. A detailed evaluation uncovered historical temporomandibular joint changes, occlusal dysfunction, and biomechanical risks stemming from extensive restorations. Using an established systematic approach, a comprehensive treatment plan was designed to address the patient’s cosmetic desires and functional issues, reduce her biomechanical risks, and create symmetrical gingival tissue to achieve a beautiful smile.
Patients often present with a chief complaint that could suggest underlying issues. In such cases clinicians may be challenged with not only developing a treatment plan to address these underlying risk factors but also effectively communicating them to the patient. The present case illustrates how a systematic approach grounded in established principles produced a comprehensive treatment plan addressing occlusal dysfunction, biomechanical risks, and esthetic goals that demonstrated to the patient the need for treating these issues. Clear aligner therapy utilizing slow orthodontic extrusion improved the appearance of the patient’s missing papilla, evened her gingival margins, and prepared the area of tooth No. 10 for a potential pontic site. Adapted centric posture was used to restore her occlusion, and cohesive restorations restored function and delivered a natural esthetic smile
Clinical Case Overview
A 52-year-old woman who was not yet an established patient at the author’s practice but intended to become one presented for a problem-focused examination with a chief complaint of a fractured mandibular right molar (tooth No. 30). A zirconia restoration was placed at that time to address the immediate concern of a fractured cusp on a large multi-surface amalgam restoration.
The patient expressed worry about further tooth fractures and dissatisfaction with anterior tooth wear and chipping (Figure 1 and Figure 2). She sought esthetic smile improvement and a comprehensive plan to prevent further breakdown and was open to a systematic approach to data gathering for diagnoses and planning. Historically reliant on single-tooth dentistry, she embraced a thorough approach that involved orthodontics and restorative care to address occlusal and esthetic issues.
Medical History
The patient had a history of hyperlipidemia managed by atorvastatin for the past 10 years. She was classified as American Society of Anesthesiologists (ASA) category II.1
Dental History
The patient had a history of extensive dental treatment that included extractions, a dental implant, root canals, post-and-core restorations, and crowns. She reported no significant issues in the past 5 years, except the recent tooth fracture of No. 30. Mild, sporadic daytime clenching was noted, but the patient denied any pain or impact on her quality of life. Esthetic concerns included tooth shape, position, and color with a history of over-the-counter whitening product use.
Clinical examination identified large restorations (>1/3 intercuspal width) and wear patterns not reported in her dental history questionnaire. Notably, anterior tooth wear was evident, but the patient felt that the wear had not changed in the past 5 years, which was supported by a 12-year historical photograph. This suggested that the occlusal damage could be a result of previous adaptation rather than active breakdown. The report of clenching, however, indicated an ongoing problem, requiring a joint-based reference position.
Diagnosis, Risk Assessment, and Prognosis
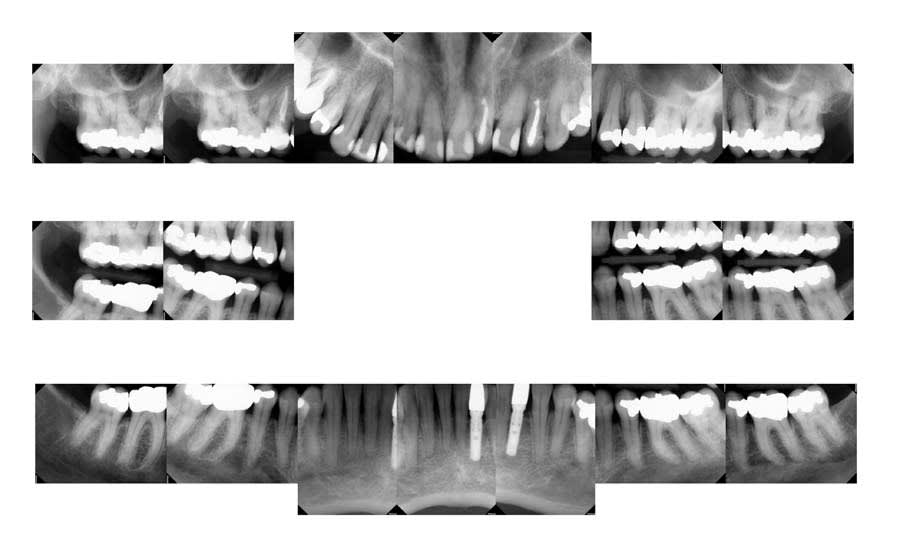
Periodontal: The patient had maintained consistent 6-month dental visits for 30 years. She presented with generalized mild recession (1 mm to 2 mm on multiple teeth), a stable free gingival graft from 20 years prior, and prescription fluoride toothpaste use. Radiographs showed generalized interproximal bone levels of 2 mm to 3 mm from the cementoenamel junction (CEJ) and probing depths of 1 mm to 3 mm, except for localized 4 mm pockets on teeth Nos. 14 and 19, mesial and distal surfaces, respectively. No mobility was noted, and there was no bleeding on probing except on the distal surface of tooth No. 3. Statin use may have reduced inflammation, supporting periodontal stability. She was classified as American Academy of Periodontology (AAP) stage II, grade A (Figure 3).2
Risk: Moderate
Prognosis: Good
Biomechanical: No active caries or xerostomia was noted, but the fractured amalgam on tooth No. 30 prompted urgent treatment. Large restorations on teeth Nos. 2, 3, 12 through 15, 18 through 20, and 31, along with large Class III composites on teeth Nos. 6 through 9, indicated structural compromises. Root canal treatment on teeth Nos. 4 and 10 (apicoectomy and post-and-core [FlexiPost®, Essential Dental Systems, edsdental.com]) and marginal fractures on teeth Nos. 5 and 12 put these teeth at even further risk. Despite the lack of symptoms, future pulpal pathology was a risk for many of the patient’s structurally compromised teeth (Figure 4 and Figure 5).
Risk: High
Prognosis: Poor
Functional: Moderate anterior attrition (1 mm to 1.5 mm) was noted, particularly on teeth Nos. 6 through 9 and 24 through 27, with no significant posterior wear or abfraction lesions. The patient reported slow progression of attrition on her front teeth that had stabilized over the past 5 years, corroborated by a historical photograph. Temporomandibular joint (TMJ) evaluation revealed a 40 mm maximum opening with slight right deviation, asymmetrical lateral movements (8 mm right and 11 mm left), and no pain or joint sounds. She had facial asymmetry as her chin point was 2 mm right of center. CBCT imaging showed a non-reducing anteriorly displaced disc in the right TMJ with osteophyte formation and reduced cortical bone, contrasting a normal left TMJ (Figure 6). Occlusal dysfunction was suspected due to her aberrant chewing pattern, which resulted in unilateral attrition and clenching. Her initial deprogramming identified the first contact on tooth No. 2 with a slide into maximum intercuspation, supporting an occlusal dysfunction diagnosis.
Risk: Moderate
Prognosis: Poor
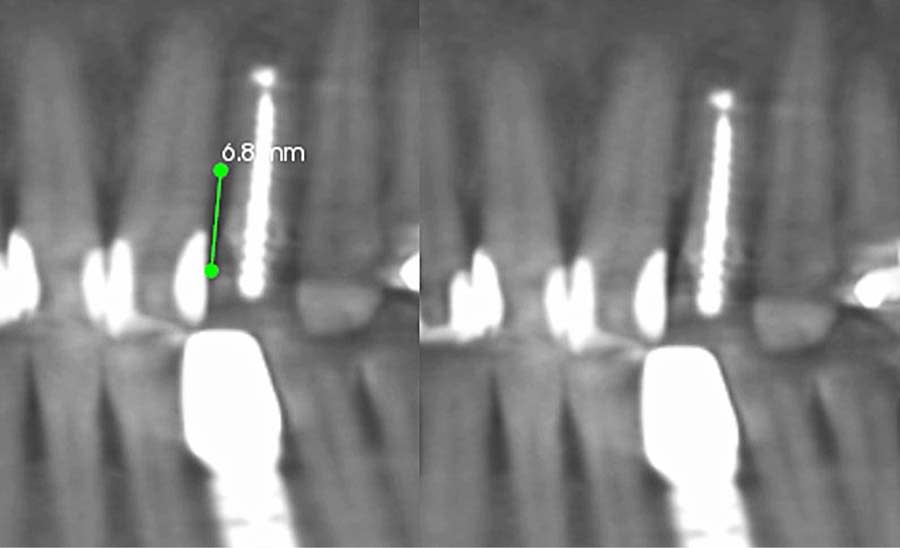
Dentofacial: The patient expressed concerns about mismatching tooth color, shape, and position. Her lip moved 10 mm from repose to Duchenne smile, placing her in the high end of normal range (6 mm to 10 mm).3 Gingival margins were uneven with supraeruption present resulting in a diagnosis of dentoalveolar extrusion with wear.4 Tooth rotations and overlaps were present as was a “black triangle,” ie, missing papilla, between teeth Nos. 9 and 10 due to the 6.8 mm distance between the crestal bone and contact point (Figure 7 and Figure 8).5 Pronounced negative buccal corridors were evident. Gingival tissue was displayed while smiling, giving the patient a high-risk dentofacial diagnosis.
Risk: High
Prognosis: Poor
Treatment Goals
The goals of treatment were to reduce biomechanical and functional risks while enhancing esthetics with a brighter, natural-looking smile. Occlusal function would be improved by addressing the aberrant chewing pattern and providing a stable occlusion in an adapted centric posture position.6 Biomechanical risk would be addressed with cohesive and adhesive indirect restorations. Esthetic goals would be achieved by leveling gingival margins, correcting dentoalveolar extrusion, addressing dark buccal corridors, and providing lighter, uniform tooth color, with improved proportions.
Treatment Plan
The treatment was phased to address high-risk biomechanical and functional issues while optimizing esthetics. In phase 1, Invisalign® treatment (Align Technology, invisalign.com) was used to align teeth, level gingival margins, and widen buccal corridors. Phase 2 involved updated diagnostics, deprogramming with a Kois deprogrammer (Kois Center, koiscenter.com), and establishing adapted centric posture. In phase 3, full-mouth rehabilitation was executed with cohesive and adhesive restorations, whitening, and resin infiltration. Phases 4 and 5 included provisional evaluation and final restoration delivery, respectively. A custom bite splint would be delivered to ensure joint stability and orthodontic retention. Periodontal health would be maintained with 6-month recare and a specific home care regimen.
Treatment Phases
Phase 1: Orthodontic Treatment
Before starting orthodontic treatment with clear aligner therapy, the option for arch expansion through orthodontics with surgical intervention (ie, surgically facilitated orthodontic therapy [SFOT] or miniscrew-assisted rapid palatal expansion [MARPE]) was discussed with the patient, which she declined. She did not report any sleep- or airway-related breathing issues and was given a low-risk status based on the STOP-BANG questionnaire and her Epworth score. However, her clinical presentation prompted further evaluation, and the patient consented to using a high-resolution pulse oximeter for 3 nights prior to the treatment planning consultation. Based on her significant oxygen desaturations, a formal sleep study was recommended to rule out obstructive sleep apnea, but the patient declined the study. To ensure adequate intraoral space, the final orthodontic and restorative plans were designed to prevent tongue space impingement and airway issues.
The use of clear aligners (Invisalign) for 12 months achieved the following:
Gingival margin leveling: Dentoalveolar extrusion and wear were addressed by intruding the maxillary anterior teeth, gingival margins were leveled relative to CEJs, and tooth No. 10 was extruded to coronally position tissue and bone (Figure 9). The latter also reduced the black triangle and maximized the predictability of the esthetics for a future pontic site, as tooth No. 10 had a guarded prognosis.7
Proportions and spacing: Oversized crowns on teeth Nos. 10 and 23 were slenderized to improve proportions for final restorations, provide space to correct anterior crowding, and create room for occlusal pathways.
Posterior uprighting: Posterior teeth were slightly uprighted to align occlusal forces, open the vertical dimension of occlusion, and widen the buccal corridors. This increase in intraoral space created more room for the patient’s tongue, decreasing airway concerns (Figure 10 and Figure 11).
Phase 2: Diagnostics, Deprogramming, Wax-up, and Bleaching
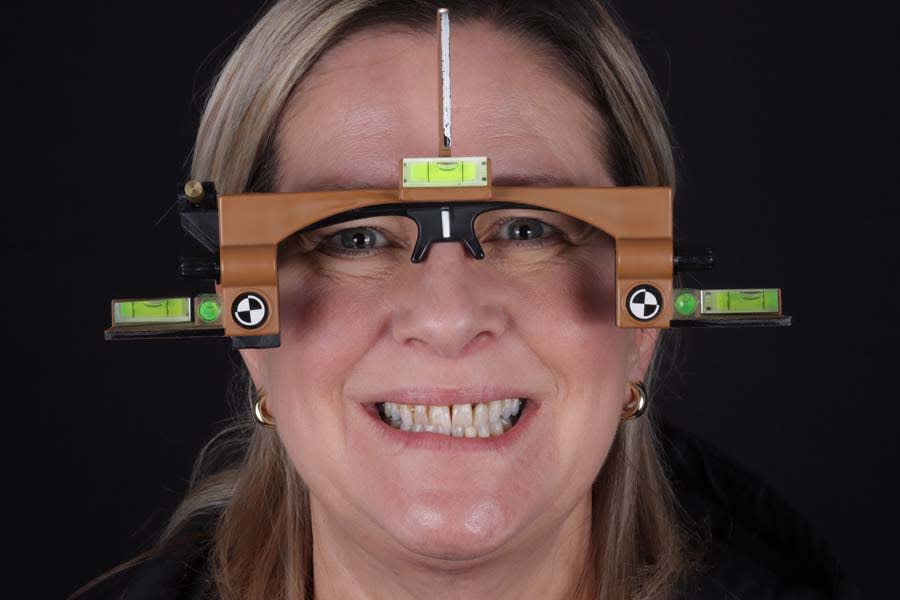
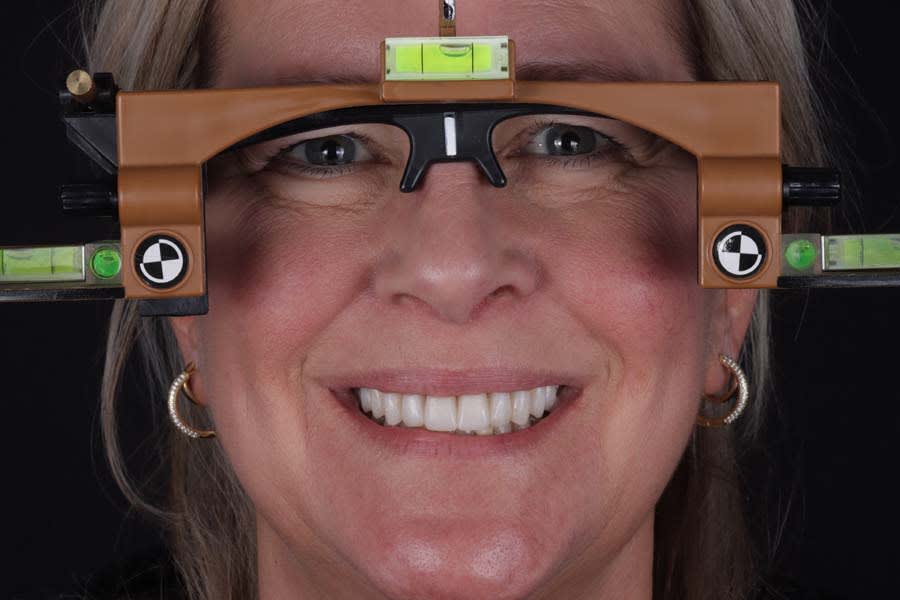
Diagnostic records were repeated post-orthodontically, including intraoral digital scans and digital intraoral and extraoral photography. Use of facial reference glasses (Kois Facial Reference Glasses, Kois Center) helped ensure that the patient’s natural head position (NHP) was recorded accurately, as many facial asymmetries were present in her interpupillary line, lip position, and facial flow (Figure 12).8 Not recording the NHP in this case could have resulted in an unwanted canted plane of occlusion in the patient’s final restorations.9 A new Kois deprogrammer was fabricated, which the patient wore for 2 weeks, and a new bite record was then taken, which, along with new intraoral digital scans, would be used to create a repeatable and comfortable bite position in adapted centric posture.
While the digital wax-up was being created, the patient began wearing her mandibular bleaching trays with 16% solution (KöR-Night™, KöR Whitening, korwhitening.com) nightly for 2 weeks. She was subsequently appointed to begin the restorative phase of her treatment.
Phase 3: Full-Mouth Rehabilitation
A full day was reserved for the patient to begin her restorative care. After local anesthetic was administered, treatment was initiated and included removing defective amalgams and composite restorations under rubber dam isolation. Preparations were cleaned using micro-abrasion (Kavo RONDOflex™, Kavo, kavo.com) with 27-micron aluminum oxide, and foundational core buildups were placed. Teeth Nos. 2 through 15, 18 through 20, 29, and 31 were prepared for lithium-disilicate crowns (IPS e.max®, Ivoclar, ivoclar.com). The porcelain-fused-to-metal crown on tooth No. 23 was removed, the existing custom abutment was utilized, and a digital scan was then taken. White spot lesions on teeth Nos. 21, 22, 27, and 28 were treated with resin infiltration (Icon Smooth Surface, DMG America, dmg-america.com).
Provisional restorations (Luxatemp®, DMG America) in shade B1 were fabricated and seated with a polycarboxylate cement (Durelon™, 3M Oral Care, 3m.com). A maxillary clear acrylic retainer was delivered for the patient to wear in the event of any chipping or breaking during the provisional phase.
Phase 4: Provisional Evaluation
One week post–provisional placement, esthetics, occlusion, and function were verified. The patient reported no complications with the provisionals and no muscle or joint pain. With the patient reclined 45 degrees, vertical contacts were checked with 12-micron red articulating paper (AccuFilm®, Parkell, parkell.com) and shimstock. Then, with the patient in an upright position, using 200-micron articulating paper (Bausch, bauschpaper.com), pathway movements were checked and any blue streaks removed.
After functional adjustment and esthetic approval, the provisionals were scanned and photographs taken for laboratory communication. Photographs included the patient wearing the facial reference glasses. The functionally and esthetically approved provisionals were then digitally scanned and digital photographs were taken, including the patient wearing the facial reference glasses in NHP. A dentofacial analyzer (Kois Dento-Facial Analyzer, Kois Center) record along with facial photographs were utilized to ensure an accurate transfer (Figure 13). Final shade photographs were taken of the unprepared and prepared teeth and the provisionals to facilitate lab communication (Figure 14).
Phase 5: Final Restoration Delivery
Provisionals were removed and the final lithium-disilicate (e.max) restorations tried in for evaluation of the esthetics by both the doctor and patient. The crowns, which were pre-etched and silanated by the lab, were cleaned after try-in using 37% phosphoric acid and silane, and the preparations were micro-abraded, rinsed, and dried. A self-adhesive resin cement (RelyX™ Unicem 2, 3M Oral Care) was tack-cured for 5 seconds and the excess cement removed. Occlusion was adjusted and verified in the same manner as the temporaries. A custom bite splint was delivered after 2 weeks, following verification of cement removal and occlusion.
Post-treatment photographs demonstrating the successful outcome of the case are shown in Figure 15 through Figure 19.
Discussion
This case highlights the efficacy of a Kois Center–based systematic approach to dental rehabilitation. Comprehensive diagnostics informed a treatment plan addressing both immediate complaints and long-term stability.
Clear aligners (Invisalign) were used to correct gingival margin discrepancies, reduce the black triangle between teeth Nos. 9 and 10, and optimize occlusal forces by uprighting posterior teeth. This orthodontic phase, paired with airway considerations, enabled functional and esthetic improvements without compromising tongue space. Establishing adapted centric posture via deprogramming created a stable occlusal scheme, thereby minimizing risks of further attrition or restoration failure. Lithium-disilicate crowns and resin infiltration restored function and delivered a natural, esthetic smile, with precise laboratory collaboration ensuring accurate shade and contour.
As in any case where there are underlying risks that are not obvious to the patient, effective patient communication was crucial. By explaining the interplay of biomechanical, functional, and esthetic risks, the clinician shifted the patient from single-tooth dentistry to embracing comprehensive care. Despite residual biomechanical risks from prior restorations, the revised occlusal scheme and high-quality materials used in this case improved the prognosis significantly while providing the patient with a beautiful smile.
Conclusion
This case exemplifies the transformative potential of a structured, systematic approach in transitioning a patient from single-tooth dentistry to comprehensive care. By addressing biomechanical, functional, periodontal, and dentofacial risks through integrated orthodontic and restorative treatments, the treatment achieved a stable, functional occlusion and an esthetically pleasing smile. The use of clear aligners, precise occlusal management, and cohesive restorations resolved immediate concerns and reduced long-term risks. Since treatment completion in early 2023, the stability of the restorations and the patient’s satisfaction have underscored the success of this approach in delivering lasting functional and esthetic outcomes.
ACKNOWLEDGMENT
The author thanks Nelson Rego, CDT, of Smile Designs by Rego for exceptional laboratory work and communication; John Kois, DMD, MSD, for his mentorship; Bill Robbins, DDS, and Jim Otten, DDS, for their guidance; and Susan Sheets, DDS, and Ken LeVos, DDS, for their support in writing this article.
ABOUT THE AUTHOR
Crystal G. Schneider, DMD, MBA
Private Practice, Mentor, Ohio
References
1. Hendrix JM, Garmon EH. American Society of Anesthesiologists Physical Status Classification System. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2025.
2. Tonetti MS, Greenwell H, Kornman KS. Staging and grading of periodontitis: framework and proposal of a new classification and case definition. J Periodontol. 2018;89 suppl 1:S159-S172.
3. Coachman C, De Arbeloa L, Mahn E, et al. Smile analysis and design in the digital era—Part I: analysis. J Cosmet Dent. 2020;36(2):
52-63.
4. Robbins JW. Differential diagnosis and treatment of excess gingival display. Pract Periodontics Aesthet Dent. 1999;11(2):265-272.
5. Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992;63(12):995-996.
6. Dawson PE. New definition for relating occlusion to varying conditions of the temporomandibular joint. J Prosthet Dent. 1995;74(6):619-627.
7. Kois JC. Esthetic extraction site development: the biologic variables. Contemporary Esthetics and Restorative Practice. 1998;2(2):1-6.
8. Silva BP, Mahn E, Stanley K, Coachman C. The facial flow concept: an organic orofacial analysis – the vertical component. J Prosthet Dent. 2019;121(2):189-194.
9. Kois JC, Kois DE, Zeitler JM, Martin J. Digital to analog facially generated interchangeable facebow transfer: capturing a standardized reference position. J Prosthodont. 2022;31(S1):13-22.