Abstract: This article presents a clinical case of a comprehensive full-mouth rehabilitation in a 26-year-old female patient with an anterior open bite and accompanying mild chronic generalized periodontitis. Contemporary digital methods involving diagnosis, modeling, and restoration fabrication were utilized. The case encompassed the use of CAD software, a Kois deprogrammer, extraction of impacted molars, cut-back technique, and artistic layering of ceramics on a lithium-disilicate framework. Significant improvements were demonstrated in both esthetics and function, with results remaining stable after 1 year of follow-up.
An open bite represents a considerably complex occlusal pathology that typically requires a multidisciplinary approach.1 Such a clinical situation is often associated not only with functional impairments but also significant esthetic challenges.2 Modern digital technologies allow for the integration of functional diagnostics, modeling, and laboratory processes to create a predictable and controlled treatment protocol.3
Lithium disilicate is among the most preferred materials for esthetic indirect restorations due to its combination of high strength, optical properties, and versatility.4 This case report, which demonstrates a comprehensive full-mouth rehabilitation utilizing lithium disilicate, emphasizes the use of the cut-back technique, multilayer ceramic application, artistic morphology detailing, and precise digital control at every stage.
Clinical Case
A 26-year-old female patient presented with complaints of unsatisfactory smile esthetics, difficulty biting food, and speech issues. Her medical history was unremarkable. Clinical examination revealed an anterior open bite, mild chronic generalized periodontitis, and impacted third molars in the third and fourth quadrants. Accurate diagnosis of occlusal issues was critical in the treatment planning.5
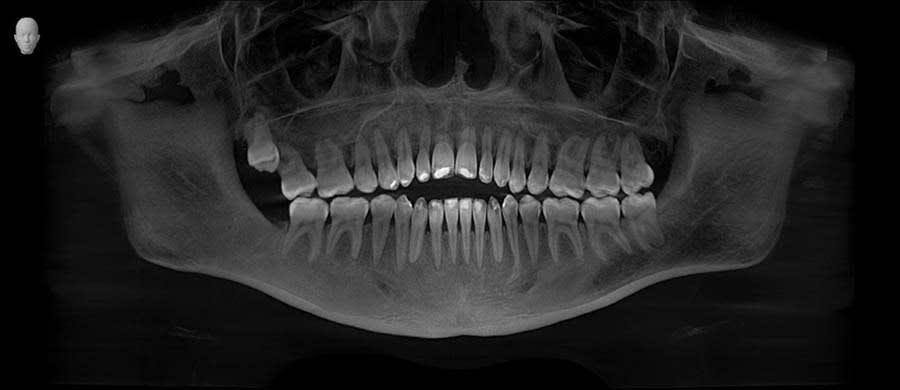
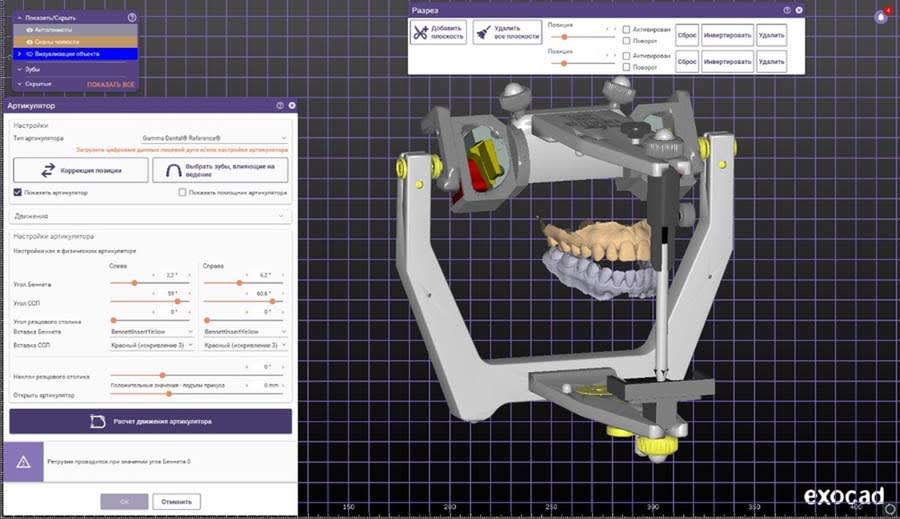
A panoramic radiograph was recorded (Figure 1), followed by a clinical examination (Figure 2). A jig was fabricated to stabilize centric relation (CR) (Figure 3), and jaw movements were analyzed using a virtual articulator in CAD software (exocad, exocad.com) (Figure 4). Digital wax-ups and guides were employed to enhance surgical and restorative accuracy.6
The diagnostic approach integrated functional, structural, and esthetic assessments. Wear patterns were evaluated, mandibular movements were analyzed, and interferences were identified. The use of a Kois deprogrammer (Kois Center, koiscenter.com) was critical in evaluating and establishing functional parameters. The patient wore the deprogrammer continuously for several days, including during sleep, allowing the masticatory muscles to relax and revealing the true neuromuscular position of the mandible. This process provided an objective functional foundation for the entire rehabilitation plan and included several key steps: an adaptation period with continuous wearing of the device; repeated evaluations of unforced mandibular closure without clinician guidance; confirmation of a consistent and reproducible CR, distinct from habitual occlusion; and the mounting of diagnostic models in CR, enabling analysis of occlusal interferences, loss of vertical dimension, and the required parameters for the proposed occlusal design. After deprogramming, a significant difference between habitual occlusion and CR was noted, confirming functional disharmony that could not be managed through localized treatment.
Articulator-mounted models in CR allowed for assessment of occlusal plane discrepancies, vertical dimension loss, compromised cusp anatomy and reduced functional pathways, and asymmetry in occlusal contacts and anterior guidance. Esthetic evaluation included analysis of smile dynamics, tooth display at rest and during speech, gingival symmetry, and proportions of the anterior dentition.
Tooth Preparation Stage
The preparation phase began after a gingivectomy procedure, which was performed using a guide based on the digital wax-up (Figure 5). Gingivectomy was carried out in advance to optimize the gingival line and prepare soft tissues for prosthetics.7 This procedure was performed in the region of teeth Nos. 6 through 11 to re-establish gingival symmetry and create proper clinical crown proportions. Prior to the gingivectomy, a periodontal evaluation, including assessment of biological width, was conducted to ensure the procedure would remain within safe biological limits.
Final clinical crown lengths were as follows: central incisors: approximately 10 mm to 10.5 mm; lateral incisors: approximately 9 mm to 9.5 mm; canines: approximately 10 mm. These measurements were based on diagnostic wax-up data, esthetic smile analysis, and functional considerations. The gingival correction provided an appropriate foundation for the definitive ceramic restorations.
After 2 weeks of healing, tooth preparation commenced. Preparation was performed under optical magnification using silicone indices derived from the wax-up (Figure 6), which helped ensure precise control of tissue reduction and adherence to the approved anatomical shape. Key parameters of tooth length, width, and proportions were documented using measuring devices and a photograph protocol prior to the procedure.
Preparation margins were rounded internally to reduce stress concentration and lower the risk of microfractures and chipping in the final restorations.8 Buccal reduction of anterior teeth was approximately 0.7 mm to allow space for multilayer ceramic application, while incisal edges were preserved to maintain the approved length. Premolars and molars were reduced 1.5 mm to 2 mm to ensure sufficient material thickness in functional contact zones. Emphasis was placed on uniform preparation, creating smooth transitions, and maintaining parallel wall alignment for optimal restoration fit. Silicone indices were used for depth control, with additional reduction performed as needed. Minimal enamel areas were preserved to avoid unnecessary tissue loss.
All prepared surfaces were refined with fine-grit diamond burs to smooth micro-irregularities, reduce chipping risks, and improve adaptation.9 Final polishing was done with soft brushes and polishing pastes to remove residual roughness and prepare for provisional restorations (Figure 7). Temporary restorations, fabricated from matrices based on the wax-up, were placed to protect prepared tissues, stabilize the gingival contour, and allow the patient to adapt to esthetic and functional changes.
During the provisional phase, clinical adjustments were made, including refining smile line parameters, lip support thickness, phonetic features, and harmony with facial soft tissues. The provisional restorations enabled critical feedback on esthetics and function (Figure 8).10 These adjustments were documented and incorporated into the final CAD design. Final documentation included photographs of prepared teeth (Figure 7), provisional restorations (Figure 9), and gingival contours to communicate with the laboratory and facilitate treatment accuracy.
Laboratory Stage
The final restoration design was created in CAD software. Based on scans of the provisionals and the approved wax-up, the final design was completed factoring in soft-tissue contours post-gingivectomy and adjustments in tooth length and proportions. Other considerations in the restoration design included the maintaining of functional occlusion from the provisional restorations and the integration of CAD articulator parameters.
All 28 restorations were milled from low-translucency lithium-disilicate blocks, shade BL3 (IPS e.max® CAD, Ivoclar, ivoclar.com). Attention was given to toolpath selection to minimize internal stress, wall thickness adherence, and preventing microcracks at incisal edges and cervical areas. Primary finishing after milling included removal of milling marks with fine diamond burs, smoothing of any sharp edges, and rounding transitions to reduce chipping risks. Fit was checked on the model to avoid tension.
Milled restorations with cut-back designs allowed for optimal esthetic layering.11 To achieve ideal esthetics and incisal translucency, cut-back entailed 0.7 mm to 1 mm buccal reduction from premolar to premolar in both arches and 1 mm incisal reduction for ceramic layering space. Care was taken to ensure smooth transitions between reduced and intact areas. Surface preparation for ceramics after cut-back included air-abrasion with aluminum oxide, ultrasonic cleaning of any residue, and silane primer application for adhesion.
Ceramic layering encompassed four main firings: base dentin layers for core color, opalescent and effect masses at the incisal zone for natural translucency, enamel with enhanced halo at the incisal edges, and, lastly, micro-relief correction and added depth in proximal zones. Each firing stage was accompanied by manual refinement to achieve natural morphology.12 Artistic refinement through post-firing adjustments included proportion corrections, individual light reflection placement per the CAD software plan, and surface texture modeling. Final glazing added gloss without masking the microtexture. Localized polishing was done with diamond pastes for controlled gloss levels (Figure 10 through Figure 12).
For quality control, each restoration underwent magnified visual inspection, fit verification on the model, articulator contact check, and post-firing crack/chip inspection. To prepare for cementation, glaze removal was done in the cementation areas, internal silane primer was applied, and individual marking was performed for clinical positioning.
Cementation Stage
Cementation was performed under rubber dam isolation following total-etch adhesive protocols,13 which included etching of enamel and dentin, priming, adhesive application, resin cementation, excess cement removal, proximal contact verification, and occlusal adjustment. Cementation of anterior restorations is shown in Figure 13.
Result
Treatment eliminated the anterior open bite, restored functional occlusion, and achieved harmonious esthetics matching the approved design (Figure 14). Final restorations showed precise proximal contacts and stable margins and required no occlusal adjustments. The multilayered lithium-disilicate restorations closely replicated natural teeth in form, color, and light dynamics.11
The esthetic result achieved anterior tooth symmetry, correct midline position, shape and proportion consistent with the approved wax-up, and individual effects like opalescence, incisal translucency, and natural halo. The patient reported significant improvement in smile esthetics, increased social confidence, and functional satisfaction. Clinical documentation confirmed no inflammatory changes at the gingival margin, stable soft tissues along the prosthetic structures, and preserved papilla height.
At 1-year follow-up, the gingival contour remained stable with no inflammation, recession, or discoloration of restorations. The long-term stability of the esthetics and function reflected the quality of the material choices and protocol adherence.13 Functional parameters were maintained, including no occlusal interferences, stable CR, and balanced lateral contacts. The patient continued using a custom nightguard to prevent potential parafunctional forces. The esthetic result, which remained unchanged after a year, demonstrated restoration durability, biocompatibility, and an effective protocol.
Final photographs showed smile harmony, optimal anterior tooth display, symmetry, and balanced soft- and hard-tissue relationships (Figure 15). The achieved outcome aligned with the initial clinical and esthetic goals and required no further corrections. The case demonstrated successful management of a complex open-bite rehabilitation through a multidisciplinary approach, digital modeling, and integrated functional diagnostics.
Discussion: Rationale for Full-Mouth Rehabilitation
While orthodontic treatment was considered during the initial diagnostic phase, and the use of either fixed orthodontic appliances or clear aligners was discussed with the patient, a comprehensive clinical evaluation dictated that orthodontics alone could not address several fundamental issues present in this case. The primary clinical reasons why an orthodontist was not part of the interdisciplinary team and why orthodontics was excluded as a definitive treatment approach included: significant generalized tooth wear and substantial loss of clinical crown height, which would require restorative intervention regardless of tooth movement; the need to re-establish an appropriate vertical dimension of occlusion, which could not be achieved by orthodontics alone; and a noticeable discrepancy between habitual occlusion and the neuromuscularly guided centric relation (centric occlusion [CO]–CR discrepancy) that was revealed after deprogramming, indicating functional disharmony.
In addition to these clinical factors, the patient declined orthodontic treatment for personal reasons, specifically citing the projected 12- to 18-month treatment duration, esthetic limitations during therapy, and her desire for a faster and definitive functional and esthetic outcome.
Before finalizing the treatment plan, various conservative alternatives were reviewed, including localized restorations, limited esthetic treatment of the anterior segment, segmental rehabilitation, and minimally invasive approaches. However, none of these conservative options were compatible with the diagnostic findings. The comprehensive diagnostic process revealed several key issues that justified full-mouth rehabilitation as the most clinically sound approach: loss of vertical dimension accompanied by significant shortening of the clinical crowns; absence of stable anterior guidance and compromised lateral guidance; pronounced wear facets indicative of parafunctional activity; and esthetic disharmony, including insufficient tooth display, a compromised smile line, and asymmetry of the gingival contour.
Localized or segmental approaches would not have restored functional stability, harmonious occlusal contacts, or proper biomechanical load distribution, nor would they have achieved the esthetic goals related to tooth proportions, symmetry, and visibility during smiling and speech. Thus, after a review of all viable treatment options, the patient provided fully informed consent and chose comprehensive rehabilitation as the most predictable and long-term solution, both functionally and esthetically.
Conclusion
This case illustrates the benefits of combining digital technologies, clinical precision, and laboratory artistry.13 The cut-back technique enabled enhanced translucency in the definitive restorations, and multilayer ceramic application provided depth and natural coloration. Success relied on precise clinician–technician collaboration and strict protocol adherence. Notably, the provisional phase played a critical diagnostic and adaptive role, minimizing final restoration adjustments.
ACKNOWLEDGMENT
The author thanks Dr. Bohdan Verbenets for clinical management and coordination and the Kazo Younique Laboratory team for their craftsmanship, technical expertise, and artistic restoration work. Thanks is also extended to the clinic staff for supporting the clinical stages, the patient for her trust, patience, and active participation, and colleagues whose consultations contributed to the success of this case.
ABOUT THE AUTHOR
Oleksandr Tierientiev, CDT
Dental Technician, V Smile Global, Los Angeles, California
References
1. Dawson PE. Functional Occlusion: From TMJ to Smile Design. St. Louis, MO: Mosby Elsevier; 2007.
2. Coachman C, Calamita MA. Digital smile design: a tool for treatment planning and communication in esthetic dentistry. Quintessence Dent Technol. 2012;35:103-111.
3. Giordano R. Materials for chairside CAD/CAM-produced restorations. J Am Dent Assoc. 2006;137(suppl):14S-21S.
4. Goodacre CJ, Garbacea A, Naylor WP, et al. CAD/CAM fabricated complete dentures: concepts and clinical methods of obtaining required morphological data. J Prosthet Dent. 2012;107(1):34-46.
5. Chu SJ, Devigus A, Mieleszko AJ. Aesthetic Restorative Dentistry: Principles and Practice. Hanover Park, IL: Quintessence Publishing; 2011.
6. Ferencz JL, Silva NRFA, Navarro JM. High-strength ceramics: clinical considerations. Compend Contin Educ Dent. 2010;31(9):682-692.
7. Edelhoff D, Sorensen JA. Tooth structure removal associated with various preparation designs for anterior teeth. J Prosthet Dent. 2002;87(5):503-509.
8. Farias-Neto A, de Medeiros FCD, Vilanova L, et al. Tooth preparation for ceramic veneers: when less is more. Int J Esthet Dent. 2019;14(2):156-164.
9. Xu HH, Kelly JR, Jahanmir S, et al. Enamel subsurface damage due to tooth preparation with diamonds. J Dent Res. 1997;76(10):1698-1706.
10. Van Meerbeek B, De Munck J, Yoshida Y, et al. Buonocore memorial lecture. Adhesion to enamel and dentin: current status and future challenges. Oper Dent. 2003;28(3):215-235.
11. Kimmich M, Stappert CFJ. Intraoral treatment of veneering porcelain chipping of fixed dental restorations: a review and clinical application. J Am Dent Assoc. 2013;144(1):31-44.
12. Pjetursson BE, Tan K, Lang NP, et al. A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. Clin Oral Implants Res. 2004;15(6):625-642.
13. Pjetursson BE, Sailer I, Zwahlen M, Hämmerle CHF. A systematic review of the survival and complication rates of all-ceramic and metal-ceramic reconstructions after an observation period of at least 3 years. Part I: single crowns. Clin Oral Implants Res. 2007;18(suppl 3):73-85.