Abstract: This study evaluates the accuracy and reproducibility of three centric relation (CR) recording techniques—bimanual manipulation (BM), chin-point guidance (CPG), and anterior deprogrammer (ADP)—using the OccluSense® (OS) digital occlusal analyzer. Addressing a critical gap in prosthodontic literature, the research employs a prospective, single-center, within-subjects design with 27 participants. Each underwent five CR registrations (BM, BM2, CPG, CPG2, and ADP) over 2 days. Statistical analyses (descriptive statistics, Cohen’s Kappa, and Fleiss’ Kappa) revealed that BM and CPG demonstrated substantial initial agreement with the ADP reference. However, reproducibility declined in repeated measurements. The ADP method exhibited superior consistency, reinforcing its role as the gold standard. Side-based agreement analysis highlighted operator dependency for manual techniques. The study concludes that while ADP remains the most reliable CR recording method, BM and CPG are viable alternatives when performed by skilled clinicians. Digital tools like OS enhance objectivity but do not replace clinical expertise.
For years, researchers have studied occlusal contacts to determine their precise location and explore various materials and methods for their registration.1,2 The establishment of a repeatable reference position for the mandible is of paramount importance in various treatments. This is especially critical in complete-arch restoration cases, with or without modification to the occlusal vertical dimension.3,4 The centric relation (CR), thus, has emerged as the most widely adopted reference point. As the only repeatable, reproducible, and recordable position for prosthesis fabrication, CR holds essential clinical significance. Typically, guiding the mandible into the CR position should be done in a physiologically reliable and unforced manner.5 A range of CR techniques has been well documented in the literature, offering diverse approaches to capture this crucial reference point.6 Surprisingly, despite the multitude of methods described in the literature, there remains a glaring absence of clinical studies that rigorously compare these techniques for recording CR.7
Recently, in this era of digital dentistry, a digital occlusal analyzer (OccluSense®, Bausch, occlusense.com) that records maxillofacial relationships in real-time, may be used to record the maxillofacial relationship and translate it into a digital format.8 This innovative tool allows all CR techniques to be applied and the results to be compared promptly.
The purpose of this study is to evaluate different CR recording techniques—anterior deprogrammer (ADP), bimanual manipulation (BM), and chin-point guidance (CPG)—using the OccluSense (OS) digital analysis device by comparing the location of occlusal contact points.
The hypothesis tested includes a null hypothesis (H0), stating that the two manipulation techniques BM and CPG provide a different maxillofacial relation recording compared to the anterior ADP and H1, proposing equivalence between these methods when analyzed with OS.
Materials and Methods
Study Design
This prospective, single-center, within-subjects study compared three CR recording techniques: BM, CPG, and ADP. Each participant underwent all techniques over two consecutive morning sessions to minimize circadian variability in neuromuscular activity. The study was approved by the Saint Joseph University (Beirut, Lebanon) Ethics Committee (Protocol #FMD-USJ-169-2024) and adhered to CONSORT guidelines for clinical trials.
Participants
A power analysis (G*Power v3.1.9.7, α = 0.05, power = 80%, effect size = 0.5) determined the sample size of 27 patients. Participants signed a written consent sheet and were informed of their right to withdraw at any time without consequences.
Inclusion Criteria
Inclusion in the study required: ≥24 natural or restored teeth; occlusal stability (no active tooth mobility or orthodontic treatment within 6 months); asymptomatic temporomandibular joints (TMJs) (ie, no pain, clicking, or restricted movement); no systemic conditions affecting TMJ function (eg, rheumatoid arthritis).
Exclusion Criteria
Exclusion from the study included: diagnosed temporomandibular disorders (TMDs); history of TMJ surgery or trauma; use of muscle relaxants or psychotropic medications.
Procedure
The prerecording protocol was as follows: Participants avoided caffeine, alcohol, and chewing 12 hours prior. Baseline relaxation entailed 15 minutes in a quiet, dimly lit room. Passive jaw stretching comprised three cycles of 10 mm opening/closing guided by the operator.
CR recording sessions were as follows:
Day 1:
- Baseline intercuspal position (ICP): habitual occlusion recorded using OS.
- Randomized techniques: BM and CPG performed in randomized order.
- BM: Operator positioned behind the patient, applying upward-backward force on the mandibular angle and chin to seat condyles.
- CPG: Operator’s thumb placed intraorally at the infradentale point, guiding mandibular closure.
- One registration per technique (BM1, CPG1), with 10-minute seated rest intervals.
Day 2:
- Repeated BM and CPG recordings (BM2, CPG2) under identical conditions.
- ADP protocol: A ready-made 2-mm thick anterior deprogrammer (AFR-Mini-Reg, Dentrade, dentrade.com) was fixed on the two maxillary central incisors using polyvinyl siloxane (Futar® Fast, Kettenbach, kettenbach-dental.us). This was done to create a unified disocclusion space between patients and reduce any biases. After 30 minutes of wear (to deprogram musculature), CR was recorded.
Outcome Variables
The first occlusal contact point (categorized into 12 segments: R1–R6, L1–L6) identified by OS.
Statistical Analysis
Statistical analysis was performed using RStudio version 2024.12.1. Descriptive statistics were used to summarize contact distribution. Agreement was assessed using raw agreement percentages, Cohen’s Kappa for pairwise comparisons, and Fleiss’ Kappa for overall agreement between methods. Reproducibility was evaluated between repeated registrations (BM1 vs BM2 and CPG1 vs CPG2). Agreement on side (right vs left) was also examined. Statistical significance was set at P ≤ .05, and Kappa values were interpreted using Landis and Koch’s scale.
Results
Descriptive Data
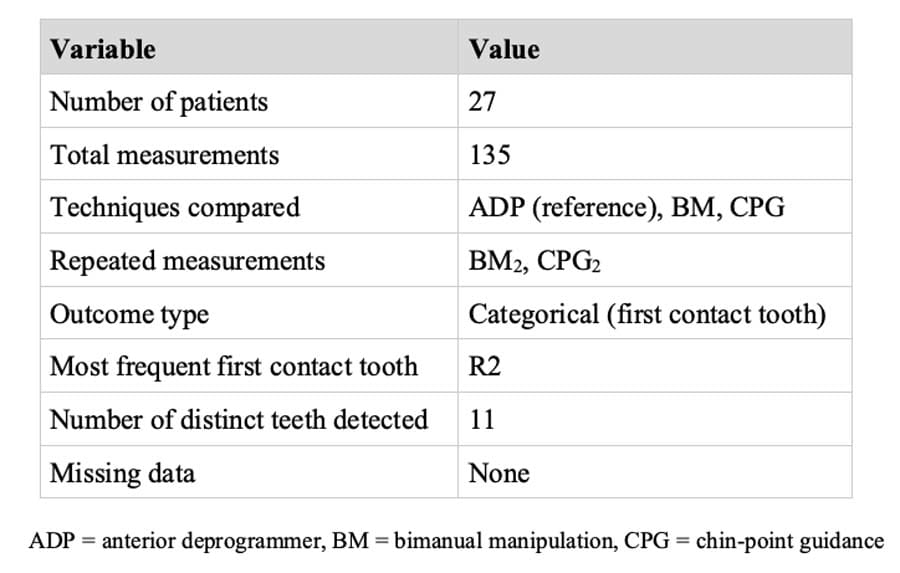
A total of 135 registrations were analyzed, corresponding to five CR recordings per patient across 27 participants (Table 1). The first point of contact was categorized by tooth (eg, “R2”), with 11 distinct teeth identified. All data were complete, with no missing values.
Raw Agreement and Reproducibility
In terms of raw agreement with the reference ADP, BM yielded the highest concordance at 74.1%, followed by CPG at 66.7% (Figure 1). When the techniques were repeated (BM2 and CPG2), agreement with the reference dropped notably, to 40.7% for BM2 and 48.1% for CPG2. Regarding reproducibility within techniques, agreement between BM1 and BM2 was 55.6%, while CPG1 and CPG2 achieved 70.4%, suggesting better internal consistency for CPG (Figure 1).
Agreement Analysis (Cohen’s and Fleiss’ Kappa)
Cohen’s Kappa analysis (Table 2) showed substantial agreement between technique BM and the reference (κ = 0.70, P < .001), and between technique CPG and the reference (κ = 0.61, P < .001). However, agreement was reduced in the repeated measurements: BM2 demonstrated fair agreement with the reference (κ = 0.32, P < .001), while CPG2 showed moderate agreement (κ = 0.40, P < .001). When assessing intra-technique reproducibility, Cohen’s Kappa revealed moderate agreement between BM1 and BM2 (κ = 0.49) and substantial agreement between CPG1 and CPG2 (κ = 0.65), further supporting the greater reproducibility of technique CPG.
To evaluate overall agreement among the three techniques, Fleiss’ Kappa was calculated using only the first measurement from each method. The resulting coefficient was 0.614 (P < .001), indicating substantial agreement across techniques beyond chance (Table 3).
Statistical Comparison and Side-Based Agreement
Despite these levels of agreement, Fisher’s exact test revealed statistically significant differences between the distribution of contact points for each technique (BM1, BM2, CPG1, and CPG2) compared to the reference (ADP), with all P values < .05. This suggests that while patterns of contact detection were similar, the techniques are not fully interchangeable with the reference method.
Finally, side-based analysis showed that techniques BM and CPG correctly matched the reference hemijaw (right vs left) in 77.8% and 81.5% of cases, respectively. In contrast, the repeated measurements showed a noticeable decline in side accuracy, with BM2 at 55.6% and CPG2 at 59.3%. Intra-technique side agreement remained consistent at 77.8% for both BM1 vs BM2 and CPG1 vs CPG2, indicating that while each technique tended to reproduce its own side preference reliably, its accuracy relative to the reference decreased upon repetition.
Discussion
The present study provides a critical evaluation of three CR recording techniques—BM, CPG, and the ADP—using the OccluSense digital occlusal analyzer. Regardless of outcomes, the study underscores the transformative potential of digital occlusal analysis in refining CR recording protocols, ultimately enhancing the predictability of prosthodontic rehabilitations. The findings reveal significant insights into the reproducibility, accuracy, and clinical applicability of these methods while addressing gaps in the literature regarding digital versus conventional CR recording protocols; thus, the null hypothesis was rejected.
The advent of digital analyzers has introduced new methodologies claiming enhanced precision, reproducibility, and integration with digital workflows.9,10 Despite these advancements, the literature reveals critical gaps in comparative studies evaluating traditional versus digital CR recording techniques.11
The study demonstrated substantial initial agreement between manual techniques BM1 and the ADP reference standard, consistent with prior studies validating operator-guided methods in controlled settings.9,10 For instance, Jász et al found the BM technique achieved minimal deviation from maximal ICP, aligning with the physiological accuracy observed here.9 However, reproducibility declined markedly during repeated measurements—a phenomenon that was also noted in studies evaluating intraoperator variability in manual techniques.1 This decline may stem from operator fatigue, subtle force application inconsistencies, or neuromuscular adaptations in patients.1
The ADP, by contrast, maintained consistency as a patient-guided technique, reinforcing its status as a gold standard. This aligns with Nuytens et al, who emphasized that patient-guided methods reduce forced condylar positioning errors common in operator-dependent techniques.12,13 Kattadiyil et al noted polyvinyl siloxane records with ADP showed higher reproducibility than Myo-monitor techniques, underscoring the ADP’s reliability.11
Conventional CR recording methods, such as BM and Gothic arch tracing, have been validated for reproducibility when performed by trained clinicians. For instance, it was demonstrated that BM and anterior deprogramming devices achieved consistent condylar positioning, whereas Myo-monitor techniques showed significant variability.14
However, these methods are inherently subjective, prone to interoperator variability, and lack quantitative data output, limiting their integration into digital workflows.15
Similar to T-Scan’s (Tekscan, tekscan.com) superiority in sensitivity over CEREC Omnicam (Dentsply Sirona, dentsplysirona.com),16 OccluSense provided high-resolution data critical for validating manual techniques.17,18 For example, Thumati et al demonstrated that digital analyzers reduce guesswork in occlusal adjustments by offering real-time force magnitude measurements.19 Similarly, Jász et al reported that digital mandibular motion analyzers could replicate CR positions with minimal deviation from the ICP, particularly when using Dawson’s BM or linguomandibular homotrophy techniques. This aligns with the current study’s use of OccluSense to objectively compare BM, CPG, and ADP outcomes.20,21
This study suggests that the ADP demonstrates superior reproducibility in complex cases such as full-arch rehabilitations and TMD management, where precision is critical to minimizing biomechanical overload and ensuring prosthetic longevity.22,23 While BM and CPG show substantial initial agreement with ADP, their declining reproducibility in repeated measurements underscores the necessity of clinician expertise, especially in critical cases requiring verification.22 The integration of digital tools like OccluSense enhances clinical training by mapping occlusal forces in real time, reducing interoperator variability and improving dynamic occlusal analysis, as seen in studies comparing digital systems to traditional methods.24
This study presents certain limitations, however. The exclusion of edentulous and TMD populations, which complicate CR determination, limits its generalizability.25,26 Additionally, while morning recordings standardized neuromuscular activity, diurnal variations in occlusal force were not assessed, potentially overlooking dynamic biomechanical stressors.24 The single-operator design, though minimizing variability, does not reflect the broader clinical reality where outcomes may vary with clinician experience, particularly in manual techniques like BM.9
Conclusion
This study addresses a key gap in prosthodontics by comparing CR recording methods using digital occlusal analysis. While ADP demonstrates superior reproducibility, bimanual manipulation and chin-point guidance remain viable when applied by skilled clinicians. Future research should prioritize diverse cohorts, integrate circadian assessments, and explore hybrid protocols combining digital analyzers with manual techniques to optimize precision and adaptability across clinical contexts.
Disclosure
The authors had no conflicts of interest to declare.
About the Authors
Abboud Youssef, DDS
Clinical Instructor, Department of Fixed Prosthodontics and Occlusion, Faculty of Dental Medicine , Saint Joseph University of Beirut, Beirut, Lebanon
Amine El Zoghby, DDS, PhD
Associate Professor and Head, Department of Fixed Prosthodontics and Occlusion, Faculty of Dental Medicine , Saint Joseph University of Beirut, Beirut, Lebanon
Camille Haddad, DDS
Assistant Professor, Department of Fixed Prosthodontics and Occlusion, Faculty of Dental Medicine , Saint Joseph University of Beirut, Beirut, Lebanon
Joseph Hobeiche, DDS, PhD
Clinical Professor, Department of Fixed Prosthodontics and Occlusion, Faculty of Dental Medicine , Saint Joseph University of Beirut, Beirut, Lebanon
References
1. Sutter B, Kerstein R, Radke J, Girouard P. A review of: “Comparison between conventional and computerized methods in the assessment of an occlusal scheme.” Adv Dent Tech. 2020;84-89.
2. Jedliński M, Mazur M, Grocholewicz K, Janiszewska-Olszowska J. 3D scanners in orthodontics—current knowledge and future perspectives—a systematic review. Int J Environ Res Public Health. 2021;18(3):1121.
3. Palaskar JN, Murali R, Bansal S. Centric relation definition: a historical and contemporary prosthodontic perspective. J Indian Prosthodont Soc. 2013;13(3):149-154.
4. El Boueiz C, Zebouni E. Full mouth rehabilitation of a combined fixed and removable prosthesis: a case report. Int Arab J Dent. 2016;7(1):article 4.
5. Galeković NH, Fugošić V, Braut V, Ćelić R. Reproducibility of centric relation techniques by means of condyle position analysis. Acta Stomatol Croat. 2017;51(1):13-21.
6. Manfredini D, Ercoli C, Poggio CE, et al. Centric relation – a biological perspective of a technical concept. J Oral Rehabil. 2023;50(11):1355-1361.
7. Thakur M, Jain V, Parkash H, Kumar P. A comparative evaluation of static and functional methods for recording centric relation and condylar guidance: a clinical study. J Indian Prosthodont Soc. 2012;12(3):175-181.
8. Bozhkova T, Musurlieva N, Slavchev D, et al. Occlusal indicators used in dental practice: a survey study. Biomed Res Int. 2021;2021:2177385.
9. Jász B, Ambrus S, Garay T, et al. Different methods of determining centric relation – comparison with a digital mandibular motion analyser. BMC Oral Health. 2024;24(1):345.
10. Revilla-León M, Agustín-Panadero R, Zeitler JM, et al. Differences in maxillomandibular relationship recorded at centric relation when using a conventional method, four intraoral scanners, and a jaw tracking system: a clinical study. J Prosthet Dent. 2024;132(5):964-972.
11. Kattadiyil MT, Alzaid AA, Campbell SD. What materials and reproducible techniques may be used in recording centric relation? Best evidence consensus statement. J Prosthodont. 2021;30(S1):34-42.
12. Nuytens P, Grande F, Li J, Lepidi L. Maxillomandibular relationship and virtual facebow integration in complete‐arch intraoral implant scan: a novel clinical technique. J Prosthodont. 2025;34(5):545-553.
13. Haddad C, Zoghbi A, Ghosn N, Youssef A. A novel 3D evaluation of the correlation between the condylar position and angle classification in a Lebanese population: a pilot study. Int Arab J Dent. 2023;14(1):article 4.
14. Kattadiyil MT, Alzaid AA, Campbell SD. The relationship between centric occlusion and the maximal intercuspal position and their use as treatment positions for complete mouth rehabilitation: best evidence consensus statement. J Prosthodont. 2021;30(S1):26-33.
15. Alghazzawi TF. Advancements in CAD/CAM technology: options for practical implementation. J Prosthodont Res. 2016;60(2):72-84.
16. Bostancıoğlu SE, Toğay A, Tamam E. Comparison of two different digital occlusal analysis methods. Clin Oral Investig. 2022;26(2):2095-2109.
17. Kerstein RB, Radke J. Clinician accuracy when subjectively interpreting articulating paper markings. Cranio. 2014;32(1):13-23.
18. Qadeer S, Ozcan M, Edelhoff D, Van Pelt H. Accuracy, reliability, and clinical implications of static compared to quantifiable occlusal indicators. Eur J Prosthodont Restor Dent. 2021;29(3):130-141.
19. Thumati P, Thumati R, Thumati PP. Understanding the influence of static and dynamic occlusal forces on the musculoskeletal system with digital occlusal analysis. In: Kerstein RB, ed. Handbook of Research on T-Scan Technology Applications in Dental Medicine. IGI Global Scientific Publishing; 2025:1723-1858.
20. Revilla‐León M, Kois DE, Zeitler JM, et al. An overview of the digital occlusion technologies: intraoral scanners, jaw tracking systems, and computerized occlusal analysis devices. J Esthet Restor Dent. 2023;35(5):735-744.
21. Lee H, Cha J, Chun YS, Kim M. Comparison of the occlusal contact area of virtual models and actual models: a comparative in vitro study on Class I and Class II malocclusion models. BMC Oral Health. 2018;18(1):109.
22. Berzaghi A, Testori T, Scaini R, Bortolini S. Occlusion and biomechanical risk factors in implant-supported full-arch fixed dental prostheses – narrative review. J Pers Med. 2025;15(2):65.
23. Youssef A, Hobeiche J, El Zoghbi A, Mortada R, Salameh Z. Bruxism and implant: where are we? A systematic review. Bull Natl Res Cent. 2022;46:172.
24. Sutter BA, Ochi L. Measuring change in first occlusal contacts from AM to PM with a digital occlusion analyzer: a pilot study. Adv Dent Tech. 2020;21-26.
25. Zheng H, Shi L, Lu H, et al. Influence of edentulism on the structure and function of temporomandibular joint. Heliyon. 2023;9(10):e20307.
26. Aoun Y, Ejbeh R, Youssef A, Hobeiche J. Salivary biomarkers as potential diagnostic tool for temporomandibular disorders: a comprehensive review. Cranio. 2025;43(4):603-612.