Robert A. Levine, DDS, FCPP, FISPPS; and Harry Randel, DMD
Abstract
A case classified as “Complex” according to the International Team for Implantology SAC (Straightforward, Advanced, Complex) classification system was treated with the Straumann® Pro Arch implant system. Management of this treatment employed a team approach to maximize the individual members’ combined knowledge to benefit the patient. The use of bone-level tapered implants, which offer good initial stability, enabled the authors to utilize immediate extraction sites while avoiding anatomic structures. Coordinated appointments and a step-by-step procedure created a positive, “seamless” experience for the patient.
The Straumann® Pro Arch solution (Straumann, www.straumann.us) provides a reliable and less com-plex treatment option for patients requiring full-arch treatments. Both patients and clinicians benefit from the combination of the individualized prosthetics and surgical advantages of the
SLActive®/Roxolid® combination. The concept of Straumann Pro Arch is based on a fixed rehabilitation that encompasses the whole procedure, from removal of hopeless teeth, immediate placement of four or more implants, and immediate loading of the implants with a fixed, screw-retained provisional. It also includes the treatment planning steps before surgery as well as afterwards when converting the temporary bridge to the final full-arch prosthesis.
Initial Situation
A periodontist and International Team for Implantology (ITI) colleague whose office is 2 hours from the authors’ practices referred a female patient whom he had recently met for the first time to the authors’ team. Initially, she was seen by the prosthodontist (Dr. Randel) and was subsequently referred to the periodontist (Dr. Levine) to develop an interdisciplinary, team approach to solve her failing dentition.
The patient presented to the authors’ offices as a 65-year-old nonsmoking woman (ASA 3; illnesses under treatment: anxiety/depression, osteoarthritis, fibromyalgia, hypothyroid, and history of myofascial pain dysfunction) (Figure 1 through Figure 3). She had a history of temporomandibular joint (TMJ) issues, including clicking and pain associated with her right side TMJ, which was presently under control and pain-free. Her chief complaint was a desire to improve her esthetics and comfort and she wanted a quick, permanent solution to replace her failing dentition. She also sought to reduce her maxillary anterior gummy smile in the final prosthesis. There was a history of parafunctional habits.
The patient had a third surgical consult with the authors for an immediate-load maxillary and mandibular hybrid restoration using the tilting of the distal implants to avoid anatomic structures of the maxillary sinus and mandibular mental foramina. This treatment concept would reduce the need for additional surgeries and the number of implants needed to provide a fixed hybrid restoration with a first molar occlusion.1,2
A medium to high lip line was noted upon a wide smile with a bi-level plan of occlusion. Also noted was supraeruption of her maxillary and mandibular anterior teeth (Nos. 7 through 10 and Nos. 25 through 27) creating a deep bite of 6 mm (Figure 2). A class I canine relationship was recorded with 6-mm overjet and 6-mm overbite. Due to her medication-induced xerostomia, generalized recurrent caries were noted. Periodontal probing depths ranged generally 4 mm to 7 mm in the maxillary jaw and 4 mm to 6 mm in the mandibular jaw with moderate to severe marginal gingival bleeding upon probing in both jaws. Tooth No. 6 was noted to have a vertical fracture clinically. There was generalized heavy fremitus in her maxillary teeth and mobilities ranging 2 to 3 degrees on the following teeth: Nos. 3, 7 through 13, 20 through 26, and 29. Her compliance profile with her previous dentists was good; however, she stated always having “issues with my gums.”
Tentative Treatment Plan
The tentative treatment plan that was discussed with the patient and her husband at the initial visit included the following:
Diagnosis: Generalized moderate to advanced periodontitis; generalized recurrent caries related to medication-related dry mouth; parafunctional habits; posterior bite collapse with loss of occlusal vertical dimension (OVD) (“mutilated dentition”).3,4
Prognosis: All remaining teeth were hopeless.
Plan: An eight-step plan was as follows:
1. Obtain a cone-beam computed tomography (CBCT) of both arches to evaluate bone quality, bone quantity, and anatomical limitations (Figure 4).
2. Articulate study models with fabrication of a diagnostic full upper denture, full lower denture, and surgical guide templates.
3. Conduct team discussions to develop the final surgical and prosthetic treatment plan for hybrid restorations using the Straumann Bone Level Tapered Implant (BLT) with a first molar occlusion. The team in this case consisted of the prosthodontist (Dr. Randel), periodontist/implant surgeon (Dr. Levine), and a representative and technician from the dental laboratory (Newtech Dental Laboratories, www.ndlsmile.com). An indirect technique would be used to fabricate the converted fixed laboratory-produced, metal-reinforced provisionals in 1 day.
4. Arrange the coordination of the surgical visit with the prosthodontist’s office and the dental laboratory. Make the patient aware that she may need to wear one or both dentures during the healing phase if the insertion torque values are not appropriate for immediate loading. This may be due to poor bone quality or quantity or the need for extensive bone grafting requiring a membrane technique for guided bone regeneration and a two-stage approach. It is important to review this with all patients particularly when only four implants are planned in the maxilla, as the distal implants(s) may record poor insertion torque values because of bone quality and quantity. Being able to use longer, tapered, and tilted implants—as in the present case with BLTs—with adequate buccal bone available for the anticipated 4.1-mm-diameter implants helps to significantly reduce this possibility.
5. Deliver the fixed provisionals in 1 day in the prosthodontist’s office.
6. Schedule postoperative visits with the periodontist’s office every 2 to 3 weeks for deplaquing, review of plaque control techniques, and delivery of a water irrigation device at 6 weeks. An occlusal adjustment should be completed at each postoperative visit with the surgical and restorative offices, because the occlusion is very dynamic as the patient’s musculature continues to accept the newly restored OVD.
7. Complete the final case at least 3 months post-surgery. In this case, because the patient will be spending the winter away in Florida, she will commence her final treatment when she returns in the spring.
8. Conduct periodontal maintenance every 3 months alternating between offices.
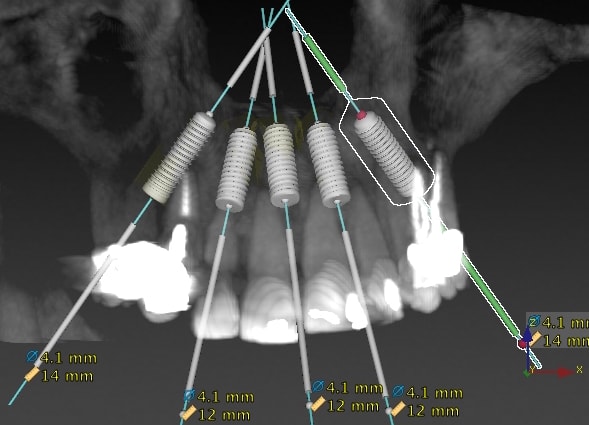
Based on CBCT analysis and the patient’s history of parafunctional habits it was decided to place five implants in the upper jaw at sites Nos. 4 (tilted), 7, between 8 and 9 (midline), 10, and 12 (tilted) after vertical bone reduction to create adequate room for prosthetics. Four implants were anticipated to be placed in the lower jaw in sites Nos. 21 (tilted), 23, 26, and 28 (tilted). The anticipated position of each implant was to be palatal to the original teeth in the maxilla and lingual to the original mandibular teeth. This would allow for screw-access holes exiting away from the incisal edges anteriorly, and, if possible, lingual to the central fossae in the posterior sextants. The palatal and lingual placement of each implant would allow their final position to be at least 2 mm to 3 mm from the anticipated buccal plates, which is beneficial for long-term bone maintenance and implant survival. If the necessary 2 mm buccal bone to the final implant position is not available, then contour augmentation (ie, bone grafting) is recommended to create that dimension. The goal is to prevent buccal wall resorption over time using slowly resorbing anorganic bovine bone (Bio-Oss®, Geistlich Biomaterials, www.geistlich-na.com) and a resorbable collagen membrane (Bio-Gide®, Geistlich Biomaterials). This membrane allows easy contouring and flexibility over the graft material when it is wet. It is also important to evaluate tissue thickness. Having at least 2 mm of buccal flap thickness over each implant is ideal, because thin tissues are associated with bone loss and recession over time.5-10
Either connective tissue grafts from the palatal flap or tuberosity can be harvested and sutured under the buccal flap. Alternatively, an allograft connective tissue or a thick collagen material (eg, Mucograft®, Geistlich Biomaterials) can be used to thicken the buccal flaps when necessary.
Surgical Appointment
The patient was premedicated with oral sedation (triazolam 0.25 mg), amoxicillin, a steroid dose pack, and chlorhexidine gluconate rinse all starting 1 hour prior to surgery. The patient’s chin and nose were marked with indelible marker, and the OVD was measured using a sterile tongue depressor with similar markings while the patient remained closed. The patient was then given full-mouth local anesthesia.
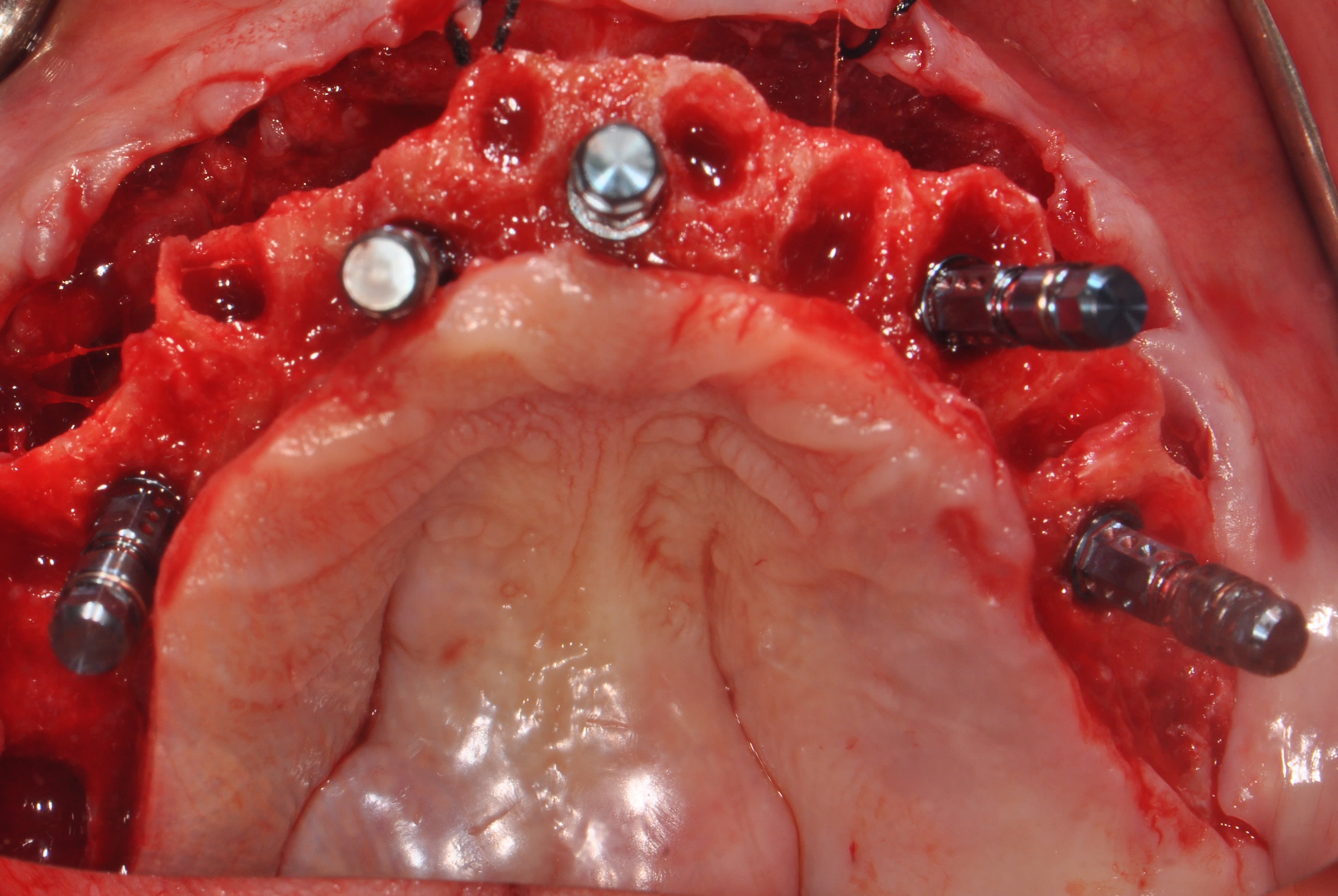
Starting with the maxillary arch, full-thickness flaps were raised and sutured to the buccal mucosa with 4-0 silk to provide improved surgical access and vision. The teeth were removed using the Piezosurgery® (Mectron, dental.mectron.com)11 with the goal of buccal plate bone preservation (using tips EX1, EX2, and micro-saw OT7S-3). The sockets were degranulated with Piezosurgery (tip OT4) and irrigated thoroughly with sterile water. With the anatomically correct surgical guide in position and being held firmly in place by the surgical assistant, measurements were made from the midbuccal of each tooth. Surgical cuts were made going from the anticipated cantilever of site No. 3 to site No. 14 using the Piezosurgery saw (tip OT7). The surgical team’s goal was to create the prosthetic space necessary, ie, 10 mm to 12 mm,12,13 for a hybrid restoration. The cuts were intentionally extended beyond the anticipated cantilever length to create adequate strength and thickness of the final prosthesis in these unsupported cantilevered areas (Figure 5 and Figure 6). The mandibular arch was treated in a similar manner. Additionally, bilateral mandibular tori reductions were accomplished with the aid of the Piezosurgery saw (tip OT7) after the extractions and prior to the vertical bone reduction of the mandibular ridge. The implants were subsequently placed.
The implant sites were prepared for the Straumann BLT implants (except for bone tapping) using the manufacturer’s protocol.14,15 The implants were placed using the surgical guide template for sites Nos. 4, 7, 8-9, 11, 13, 21, 23, and 26 with insertion torques measured at 35 Ncm; No. 28 recorded a 20-Ncm insertion torque value. All implants were 4.1 mm in diameter and 14 mm in length except for Nos. 7, 8-9, and 11, which were 12 mm in length (Figure 7). All 17- and 30-degree-angled implants were bone-profiled prior to screw-retained abutment placement. This allowed the complete seating of the screw-retained abutment at the recommended 35 Ncm torque. Using the available Straumann bone profilers with the appropriate Regular Connection (RC) inserts was a critical step for correct abutment fit. The following screw-retained abutments (all were 2.5-mm gingival heights) were then chosen: straight for Nos. 23 and 26; 17 degrees for Nos. 4, 7, and 8-9; 30 degrees for Nos. 11, 13, 21, and 28. Tall protective healing caps were then placed (Figure 8), and the dentures were evaluated to ensure there was adequate space for the pink acrylic to allow for bite registration material thickness.
All sockets and buccal gaps to the immediately placed implants were bone grafted. Prior to suturing, the tissue flaps were scalloped with 15c blades to reduce overlap of the flaps over the protective caps. This not only aided in postoperative healing but also in the restorative dentist’s visualization of the abutments for the provisional insertion. The patient was sutured with resorbable 4-0 chromic gut and 5-0 Vicryl™ sutures (Ethicon, www.ethicon.com) and released to be seen immediately by the prosthodontist for the coordinated restorative visit. The prosthodontist’s responsibilities, as will be discussed below, include bite registration, impressions, and the dental lab conversion of the complete denture to a metal-reinforced fixed transitional prosthesis (indirect provisionalization technique).
The authors’ team of restorative dentists has been treating full-arch immediately loaded cases on five to eight implants (depending on whether the restoration is a hybrid or crown-and-bridge) since 1994. Based on experience, the team presently uses the indirect technique, which is easier for everyone involved—particularly the patient. The team handles the coordinated visits between offices, the dental lab, and the implant supplier representative weeks in advance so everyone is in sync with regard to timing. These coordinated efforts could be compared to a symphony orchestra, in which all the musicians know their specific part and when and where they are expected to be. Many of the authors’ patients have described this fluidity as a seamless experience that they witness firsthand and greatly appreciate.
Same-Day Restorative Appointment With the Prosthodontist
Coming from the periodontist’s office, the patient was seen by the prosthodontist for restorative records in preparation for immediate load protocol. The previously processed dentures were first checked with pressure paste to ensure there was no contact of the intaglio surface with the tall healing caps. Bite registration material was then used to confirm there was no contact (Figure 9) and later would be used by the laboratory to articulate the models. Efforts were made to confirm the OVD (using the marked tongue depressor provided by the periodontist), incisal position, midline, plane of occlusion, and centric position with the prostheses in place. Adjustments were made as needed. Photographs were taken to document and relay information via email to the laboratory technician. The lab will use the registration material left in the intaglio surface of the prostheses, as healing caps will be placed on the newly fabricated models. This will allow the index to transfer the OVD and centric relationships with contact just on the healing caps. The soft tissue plays no role in this relationship.
A bite registration was made to confirm centric relation. Healing caps were then removed and open-tray impression copings were placed. If the connection between the implant abutments and the impression copings cannot be visualized, then x-ray confirmation of the connection is needed. Transfer impressions were made using a custom tray and rigid impression material of choice, in this case polyether. The authors’ lab courier delivered the dentures and impressions to the laboratory for the conversion to metal-reinforced, screw-retained provisionals, which would be delivered back to the restorative office within 24 hours.
The next afternoon, the prostheses were inserted (Figure 10) and panoramic radiographic confirmation of proper seating was obtained (Figure 11). Any necessary occlusal adjustments were then completed. The patient was given written instructions to be on a very soft diet for the first 4 weeks, after which a normal diet could resume. The patient was then seen every 2 to 3 weeks for deplaquing and plaque control review, per the protocol outlined earlier. The occlusion was also refined as needed. The patient was given a water irrigation device and reviewed at 6 weeks post-surgery.
Because the patient was away in Florida for the winter and unable to come in for the typical 3-month follow-up protocol, she was seen 4-1/2 months after surgery. At that time, periapical x-rays of each implant were taken to confirm bone healing. The prostheses were removed and cleaned. GC resin (GC America, www.gcamerica.com) verification jigs (Figure 12 and Figure 13), made on the original models and fabricated prior to the appointment, were tried in. If passivity is not confirmed, then the jig can be cut and re-indexed. Once the fit of the verification jigs was confirmed, custom trays were used to transfer the relationships. At the following appointments, OVD and centric relations were obtained, and the wax try-ins were confirmed for esthetics, phonetics, and occlusion prior to the milling of the framework (Figure 14). Tooth location should be confirmed prior to milling the framework so it can be designed within the parameters of the acrylic/tooth borders.
At the insertion appointment, the healing caps were removed and cleaned with chlorhexidine. Once the prosthesis was inserted, the esthetics, phonetics, and OVD were confirmed, and the occlusion adjusted as needed. Screws were tightened to 15 Ncm and screw-access openings were filled with Teflon tape to within 2 mm of the surface. A soft material such as Telio® or Fermit™ (Ivoclar Vivadent, www.ivoclarvivadent.com) can be used to seal the access. A maxillary acrylic nightguard was fabricated to aid in protecting the occlusal surfaces from wear and to help reduce any parafunctional habits. Figure 15 through Figure 18 show the completed case.
At subsequent appointments, the occlusion was evaluated and the prostheses were examined to determine if they needed to be reduced or recontoured. Eventually, the soft material used to close the access was replaced with a hard composite material over Teflon tape, which protects the screw heads.
Conclusion
A case classified as “Complex” according to the ITI SAC (Straightforward, Advanced, Complex) classification system16 and treated with Pro Arch was presented. Management of this treatment utilized the advantages of the team approach to maximize the team members’ combined knowledge to benefit the patient, consistent with ITI doctrine.17 The use of BLT implants, which offer good initial stability, gave the authors the confidence to not only use immediate extraction sites (type 1 implant placement) but also avoid anatomic structures. In this case, the structures included the maxillary sinuses, nasopalatine, and mental foramina, as well as the inferior alveolar nerve canals. In addition, with the tapered design of the BLT implants, the surgeon could utilize maxillary anterior areas to avoid apical fenestrations where undercuts could become problematic if straight-walled bone-level implants were used. The coordinated appointments, along with the symphony-like steps in the procedure, created a positive, “seamless” experience for the patient.
About the Authors
Robert A. Levine, DDS, FCPP, FISPPS
Diplomate, American Board of Periodontology; Fellow, International Team for Implantology (Basel, Switzerland); Private Practice at the Pennsylvania Center for Dental Implants & Periodontics, Philadelphia, Pennsylvania; Clinical Professor in Periodontics & Implantology, Kornberg School of Dentistry, Temple University, Philadelphia, Pennsylvania
Harry Randel, DMD
Fellow, International Team for Implantology (Basel, Switzerland); Private Practice in Prosthodontics & Advanced Restorative Dentistry, Philadelphia, Pennsylvania
The authors wish to acknowledge the work of Michael Borio, Dental Technician, Newtech Dental Laboratories, Lansdale, Pennsylvania, in this case.
All product information has been provided by the manufacturer.
References
1. Malo P, de Araújo Nobre M, Lopes A, et al. A longitudinal study of the survival of All-on-4 implants in the mandible with up to 10 years of follow-up. J Am Dent Assoc. 2011;142(3):310-320.
2. Malo P, de Araújo Nobre M, Lopes A, et al. “All-on-4” immediate-function concept for completely edentulous maxillae: a clinical report on the medium (3 years) and long-term (5 years) outcomes. Clin Implant Dent Relat Res. 2012;14 suppl 1:e139-e150.
3. Amsterdam M. Periodontal prosthesis: Twenty-five years in retrospect. Alpha Omegan. 1974;67(3):8-52.
4. Amsterdam M. Periodontal prosthesis: Twenty-five years in retrospect. Part II. Occlusion. Compend Contin Educ Dent. 1984;5(4):325-334.
5. Chen ST, Buser D. Esthetic outcomes following immediate and early implant placement in the anterior maxilla—a systematic review. Int J Oral Maxillofac Implants. 2014;29 suppl:186-215.
6. Levine RA, Huynh-Ba G, Cochran DL. Soft tissue augmentation procedures for mucogingival defects in esthetic sites. Int J Oral Maxillofac Implants. 2014;29 suppl:155-185.
7. Morton D, Chen ST, Martin WC, et al. Consensus statements and recommended clinical procedures regarding optimizing esthetic outcomes in implant dentistry. Int J Oral Maxillofac Implants. 2014;29 suppl:216-220.
8. Linkevicius T, Apse P, Grybauskas S, Puisys A. The influence of soft tissue thickness on crestal bone changes around implants: a 1-year prospective controlled clinical trial. Int J Oral Maxillofac Implants. 2009;24(4):712-719.
9. Puisys A, Virdasiute E, Linkevciene L, Linkevicius T. The use of acellular dermal matrix membrane for vertical soft tissue augmentation during submerged implant placement: a case series. Clin Oral Implants Res. 2015;26(4):465-470.
10. Levine RA, Ganeles J, Gonzaga L, et al. 10 keys for successful esthetic-zone single immediate implants. Compend Contin Educ Dent. 2017;38(4):248-260.
11.Thomas J. Piezoelectric ultrasonic bone surgery: benefits for the interdisciplinary team and patients. Functional Esthetics & Restorative Dentistry. 2008;2(3):20-24.
12. Sadowsky SJ. The implant-supported prosthesis for the edentulous arch: design considerations. J Prosthet Dent. 1997;78(1):28-33.
13. Bidra AS. Three-dimensional esthetic analysis in treatment planning for implant-supported fixed prosthesis in the edentulous maxilla: review of the esthetics literature. J Esthet Restor Dent. 2011;23(4):219-236.
14. Levine R. Advanced surface and material enable Straumann’s bone level implants to overcome placement challenges. Compend Contin Educ Dent. 2015;36(8):628.
15. Cochran D, Stavropoulos A, Obrecht M, et al. A comparison of tapered and nontapered implants in the minipig. Int J Oral Maxillofac Implants. 2016;31(6):1341-1347.
16. Dawson A, Chen S, eds. The SAC Classification in Implant Dentistry. Berlin: Quintessence Publishing; 2009.
17. Wismeijer D, Buser D, Belser U, eds. ITI Treatment Guide Vol. II. Loading Protocols in Implant Dentistry - Partially Dentate Patients. Berlin: Quintessence Publishing; 2007.