Kay Vietor, Dr med dent
Abstract
Unfavorable narrow space conditions are often found in young patients. In the case presented, after several years of orthodontic treatment a 19-year-old patient who had tooth agenesis presented with limited gap widths and poor interradicular spacing in his maxillary anterior dentition. With the aid of cone-beam computed tomography and a 3D surgical drilling template, two Straumann small-diameter Bone Level Tapered implants were used as the basis for restoration of the lateral incisors. Despite the limited gap widths and adverse interradicular spacing, an excellent outcome was achieved.
A healthy, nonsmoking, 19-year-old male patient presented with tooth agenesis of teeth Nos. 7 and 10 (Figure 1 and Figure 2). He underwent orthodontic treatment from August 2005 through September 2009 due to progeny tendency with a removable orthodontic appliance. Treatment with fixed orthodontic appliance was performed from November 2013 through April 2016.
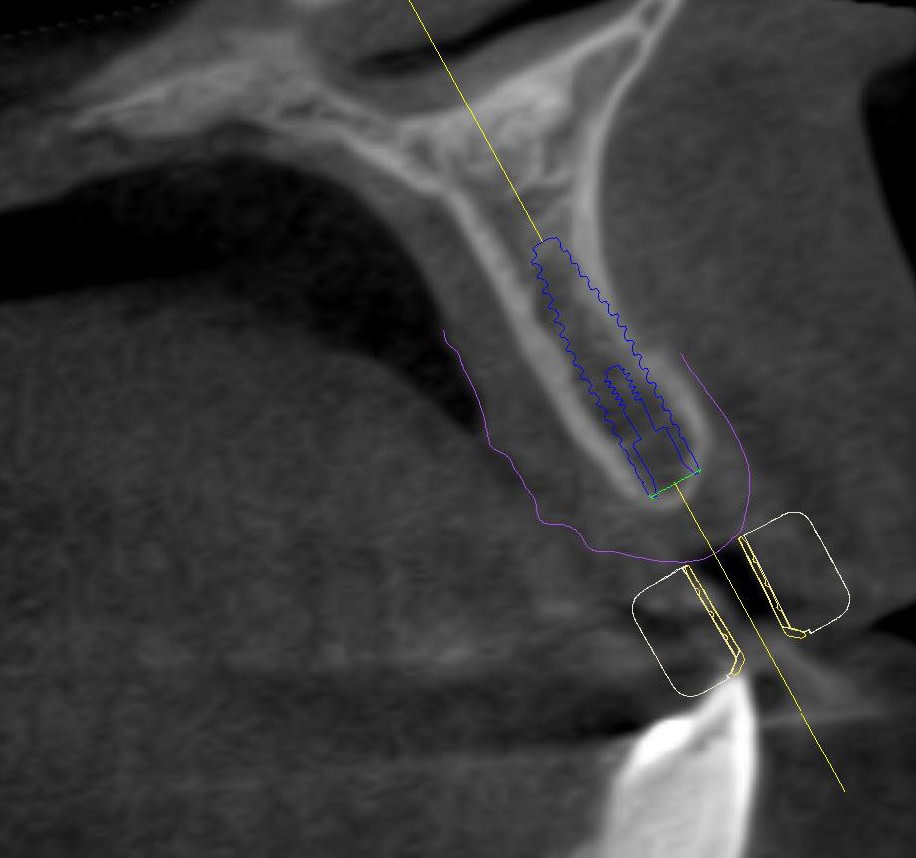
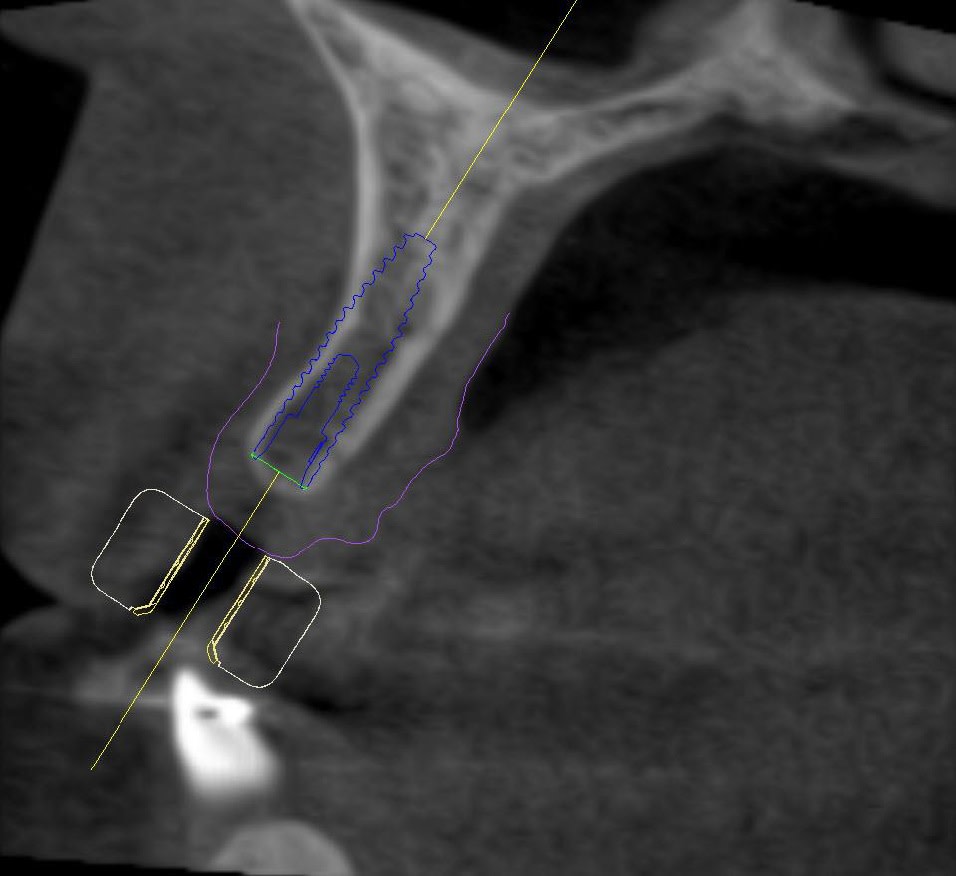
Upon completion of the orthodontic therapy, the gaps between the roots of the adjacent teeth and the crowns of the adjacent teeth were restored. The patient was showing very limited gap widths and unfavorable interradicular space conditions. Initial marginal bone thickness in the gaps was approximately 4.5 mm (Figure 3) with apical thinning (Figure 4 and Figure 5).
Treatment Planning
After discussing the treatment plan with the patient it was agreed upon that two small-diameter (2.9 mm) implants would be placed in positions 7 and 10, followed by fixed restorations. The position of the implants was carefully assessed using a cone-beam computed tomography (CBCT) technique (Figure 4 through Figure 6), and a 3D surgical drilling template was developed and printed to facilitate the drilling process (Figure 7 and Figure 8). Postoperative temporary prostheses were created to avoid gingival pressure and to secure the position stability of the adjacent teeth (Figure 9).
Surgical Procedure
Implant placement was done with the patient under local anesthesia. The implant bed preparation was performed by means of a 3D-perforated surgical drilling template. Two small-diameter implants (Bone Level Tapered [BLT], SLActive®/Roxolid®, 2.9 mm x 12 mm, Straumann, www.straumann.us) were placed in positions 7 and 10 using an open-flap technique (Figure 10), followed by bone augmentation by means of autologous bone chips and bone xenograft. Collagen membranes and apical titanium pins were used to stabilize the augmented regions, and respective protective caps were placed on the abutment portion of each implant. The flap was repositioned and the wound was closed with stress-free, tight sutures (Figure 11).
The patient was prescribed with antibiotic (2x 600-mg Clindamycin for 7 days) and anti-inflammatory (Ibuprofen 400 mg) therapy. Exact positioning of implants was further controlled and confirmed using ultra low-dose CBCT technique (Figure 12 and Figure 13).
Prosthetic Procedure
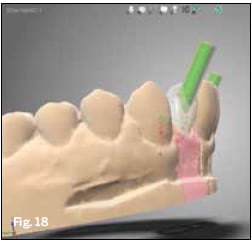
After 9 weeks of healing, minimal surgical invasion (ie, puncture incision and displacement of the tissue) in positions 7 and 10 was performed, healing screws (SC H3.5) were placed (Figure 14), and an impression was taken to produce temporary crowns for better gingiva formation and profiling (Figure 15). Following separate impression-taking (Figure 16 and Figure 17) individual restorations were designed with Straumann CARES® Visual Software 10.1 (Figure 18), produced (Figure 19), and placed.
Final Result
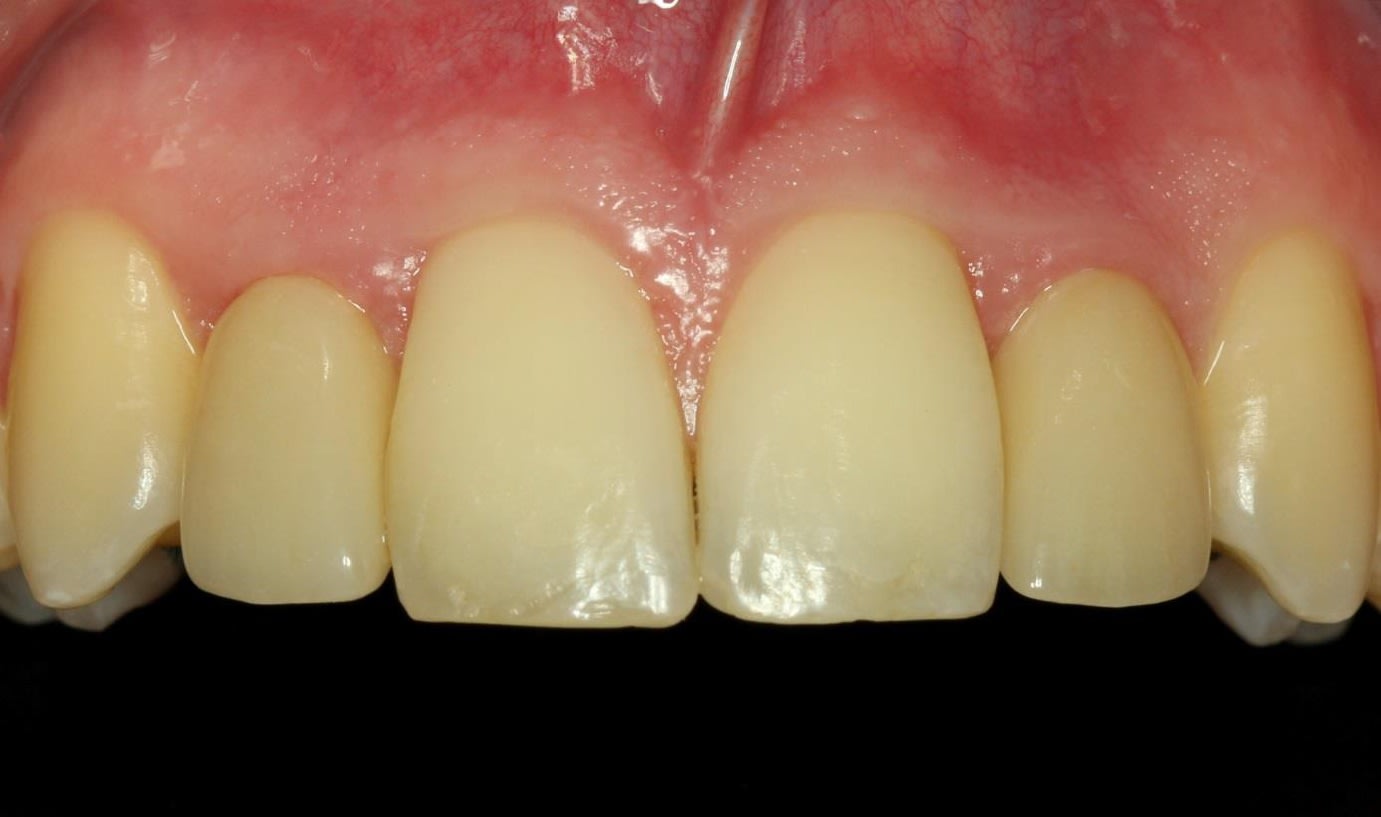
Both the patient and practitioner were satisfied with the extraoral and intraoral appearance after treatment. This was manifested by superb gingival development and good pink/white esthetics (Figure 20 and Figure 21). Despite the initial very limited gap widths and the unfavorable interradicular space conditions, the final result was excellent.
Conclusion
The Straumann small-diamter BLT 2.9-mm implant represents an enrichment of the author’s treatment portfolio that greatly simplifies treatment procedures in cases with unfavorable narrow space conditions, often found in young patients.
About the Author
Kay Vietor, Dr med dent
Private practice for oral surgery and Implantology in Langen, Germany; Post-graduate education and degree in Oral Surgery; Fellow, International Team for Implantology, Basel, Switzerland