Yong-Han koo, DDS
Diplomate, American Board of Oral and Maxillofacial Surgery; Private Practice, Wayland, Massachusetts
Key Takeaway Points
Digital workflow allows patients to be actively engaged in their treatment planning process, enabling them to grasp realistic expectations of their treatment plan prior to committing to any procedures.
Having superior diagnostic tools and the ability to execute a plan accordingly with precision is paramount.
A team approach focusing on sound fundamental principles and scientific evidence guided by advanced digital technologies brings clarity, simplicity, and efficiency, resulting in optimal, predictable outcomes with long-term stability.
Guided bone and tissue regeneration techniques have revolutionized clinicians’ abilities to treat a wide array of clinically challenging situations, ranging from mild to severe bone and soft-tissue defects. However, complications still often occur in severely compromised, complex cases. Typically, there are two main reasons: failure to diagnose properly, and an inability to execute the plan with precision. In this case, the patient unfortunately was struck by a motor vehicle while crossing a crosswalk and sustained multiple complex maxillofacial injuries. A comprehensive, staged approach utilizing advanced digital technologies (GALILEOS FaceScanner and CEREC®, Sirona Dental, Inc., www.sirona.com) led to a functional and esthetic outcome in a minimally invasive manner with high predictability. The case demonstrates the importance of satisfying the following key elements for long-term stability: placement of a 3-dimensionally sound dental implant based on an ideal restorative plan; greater than 2 mm buccal bone and 2-3 mm keratinized gingival tissue.
1. A 28-year-old female pedestrian was struck by a motor vehicle while crossing a crosswalk.
2 and 3. The patient sustained multiple complex maxillofacial injuries: orbital floor fracture; fractures of teeth Nos. 7 and 9; complete avulsion of tooth No. 8; complete labial plate dehiscence; significant loss of gingival architecture; and multiple contusions. GALILEOS CBCT (Sirona Dental, Inc.) was used in the diagnosis.
4. Retracted view, 3 months following the accident with temporization. Conservative initial surgical debridement was performed in order to avoid a collapse of both the alveolar ridge and soft tissue. There was no significant osteoclastic activity from the initial trauma at this time. Intentional endodontic therapy was rendered on teeth Nos. 7 and 9.
5 and 6. Ridge augmentation was completed with the use of a tenting screw (KLS Martin, www.klsmartin.com), recombinant human bone morphogenetic protein-2 (rhBMP-2) (Medtronic, www.medtronic.com), plasma rich in growth factors (PRGF-Endoret®) (BTI, www.bti-biotechnologyinstitute.com), collagen membrane, and a mixture of cortico-cancellous allograft and xenograft.
7. 4 months postoperative.
8 and 9. Esthetic re-evaluation with an ideal fixed temporary provisional. Significant soft tissue defects were noticed. (Fig 8 and Fig 9 courtesy of William Heggerick, DDS, prosthodontist, and Yuki Momma, RDT, Weston, Massachusetts)
10. Alveolar width increase from 1 mm to 8 mm was evident at the crest.
11. Subepithelial connective tissue graft.
12 and 13. Incorporation of an ideal fixed temporary provisional into a digital implant proposal (reverse engineering concept via CEREC, Sirona Dental, Inc.).
14. After obtaining 3-dimensionally sound implant position (3 mm from the free gingival margin and 2 mm palatal from the incisal edge), CBCT guided surgery (as shown) was performed (Classic Guide, Sirona Dental, Inc.).
15. 3-mm healing abutment was placed in order to provide a “framework” for epithelization to occur coronally (semi-submerged technique).
16 and 17. CBCT revealed 3-dimensionally sound implant placement No. 8; for optimum esthetic outcome, only a single implant for No. 8 was placed cantilevering pontic No. 7, avoiding central-lateral esthetic dilemma.
18. Patient’s smile at 1.5-year follow-up.
19. GALILEOS FaceScanner.
20. Full view at 1.5-year follow-up. (Fig 20 courtesy of Dr. Heggerick and Mr. Momma)

Figure 1
Figure 1 A 28-year-old female pedestrian was struck by a motor vehicle while crossing a crosswalk.

Figure 2
Figure 2 The patient sustained multiple complex maxillofacial injuries: orbital floor fracture; fractures of teeth Nos. 7 and 9; complete avulsion of tooth No. 8; complete labial plate dehiscence; significant loss of gingival architecture; and multiple contusions. GALILEOS CBCT (Sirona Dental, Inc.) was used in the diagnosis.

Figure 3
Figure 3 The patient sustained multiple complex maxillofacial injuries: orbital floor fracture; fractures of teeth Nos. 7 and 9; complete avulsion of tooth No. 8; complete labial plate dehiscence; significant loss of gingival architecture; and multiple contusions. GALILEOS CBCT (Sirona Dental, Inc.) was used in the diagnosis.

Figure 4
Figure 4 Retracted view, 3 months following the accident with temporization. Conservative initial surgical debridement was performed in order to avoid a collapse of both the alveolar ridge and soft tissue. There was no osteoclastic activity at this time. Intentional endodontic therapy was rendered on teeth Nos. 7 and 9.
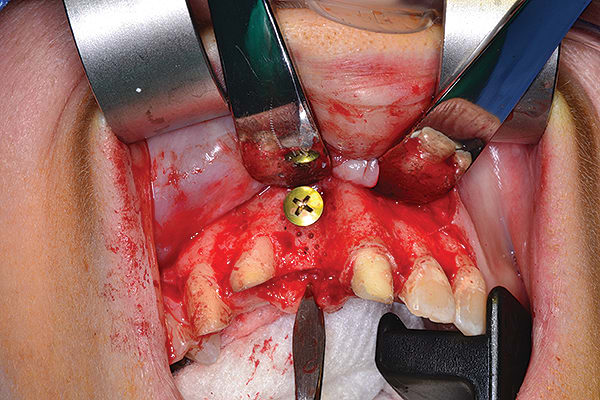
Figure 5
Figure 5 Ridge augmentation was completed with the use of a tenting screw (KLS Martin, www.klsmartin.com), recombinant human bone morphogenetic protein-2 (rhBMP-2) (Medtronic, www.medtronic.com), plasma rich in growth factors (PRGF) (BTI, www.bti-biotechnologyinstitute.com), collagen membrane, and a mixture of cortico-cancellous allograft and xenograft.
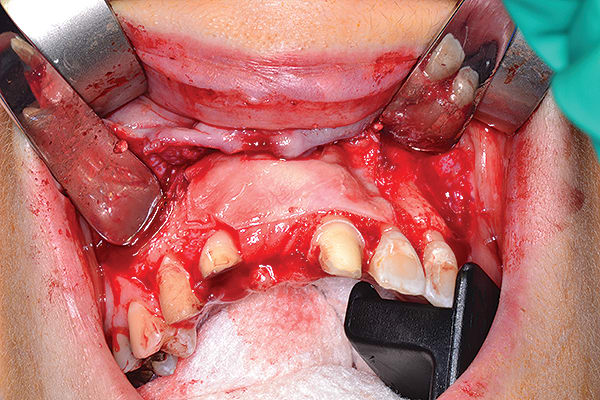
Figure 6
Figure 6 Ridge augmentation was completed with the use of a tenting screw (KLS Martin, www.klsmartin.com), recombinant human bone morphogenetic protein-2 (rhBMP-2) (Medtronic, www.medtronic.com), plasma rich in growth factors (PRGF) (BTI, www.bti-biotechnologyinstitute.com), collagen membrane, and a mixture of cortico-cancellous allograft and xenograft.

Figure 7
Figure 7 4 months postoperative.

Figure 8
Figure 8 Esthetic re-evaluation with an ideal fixed temporary provisional. Significant soft tissue defects were noticed. (Fig 8 and Fig 9 courtesy of William Heggerick, DDS, prosthodontist, and Yuki Momma, RDT, Weston, Massachusetts)

Figure 9
Figure 9 Esthetic re-evaluation with an ideal fixed temporary provisional. Significant soft tissue defects were noticed. (Fig 8 and Fig 9 courtesy of William Heggerick, DDS, prosthodontist, and Yuki Momma, RDT, Weston, Massachusetts)
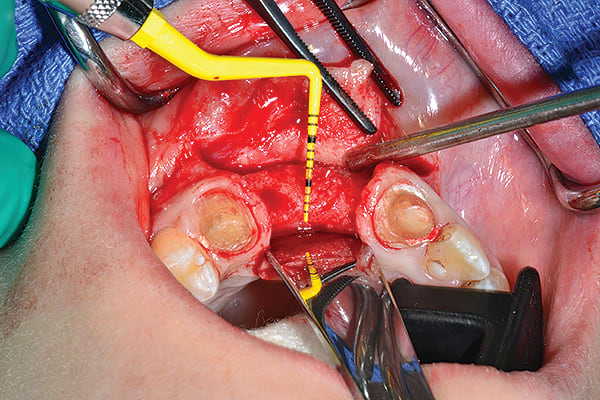
Figure 10
Figure 10 Alveolar width increase from 1 mm to 8 mm was evident at the crest.
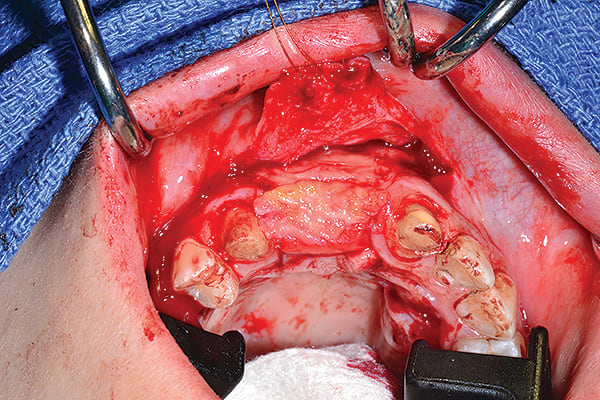
Figure 11
Figure 11 Subepithelial connective tissue graft.
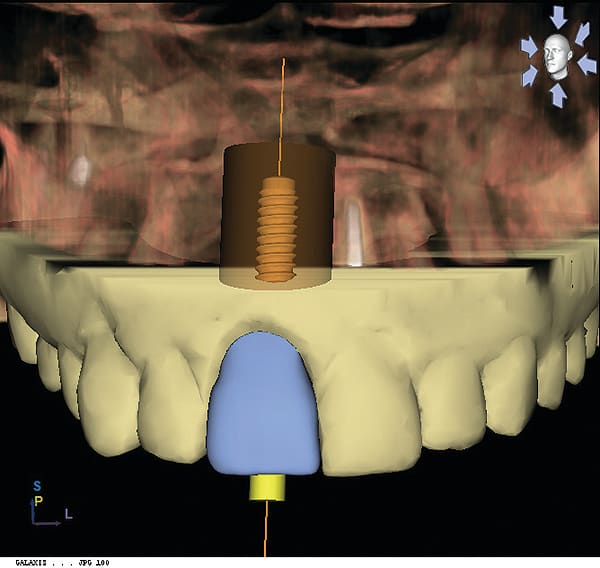
Figure 12
Figure 12 Incorporation of an ideal fixed temporary provisional into a digital implant proposal (reverse engineering concept via CEREC, Sirona Dental, Inc.).
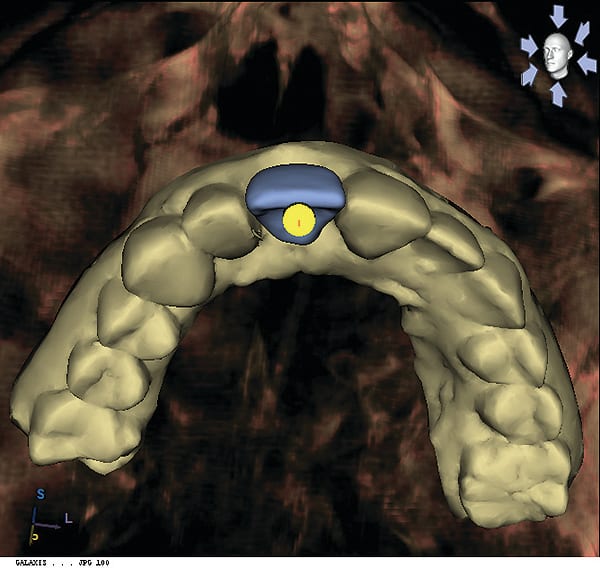
Figure 13
Figure 13 Incorporation of an ideal fixed temporary provisional into a digital implant proposal (reverse engineering concept via CEREC, Sirona Dental, Inc.).
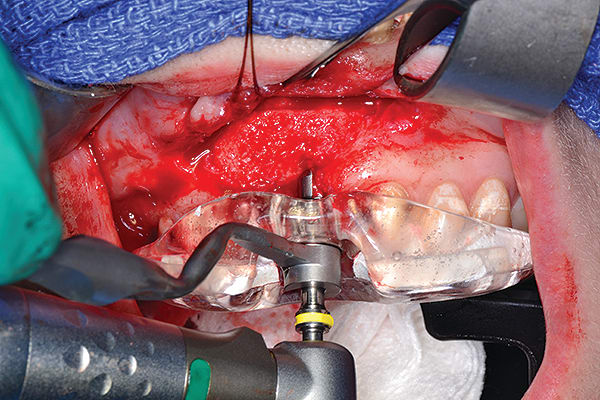
Figure 14
Figure 14 After obtaining 3-dimensionally sound implant position (3 mm from the free gingival margin and 2 mm palatal from the incisal edge), CBCT guided surgery (as shown) was performed (Classic Guide, Sirona Dental, Inc.).
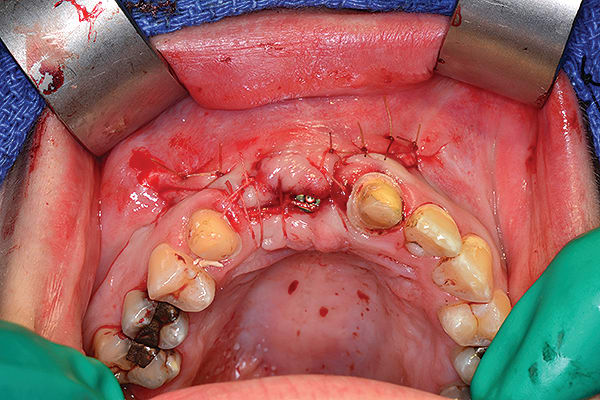
Figure 15
Figure 15 3-mm healing abutment was placed in order to provide a “framework” for epithelization to occur coronally (semi-submerged technique).
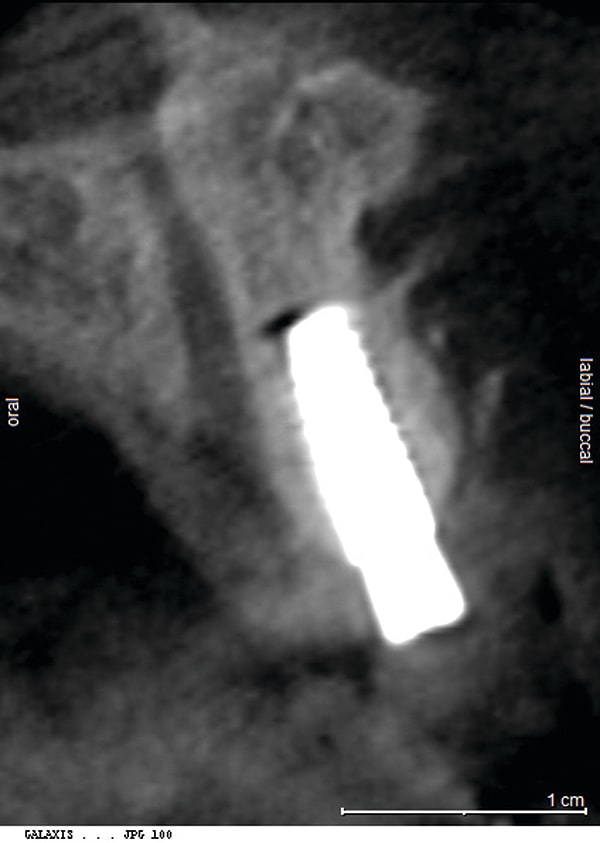
Figure 16
Figure 16 CBCT revealed 3-dimensionally sound implant placement No. 8; for optimum esthetic outcome, only a single implant for No. 8 was placed cantilevering pontic No. 7, avoiding central-lateral esthetic dilemma.
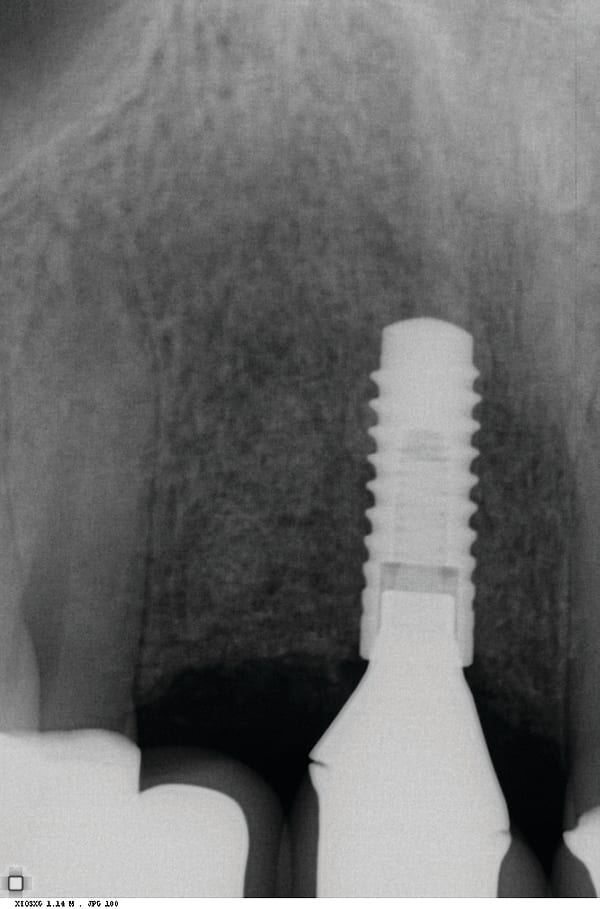
Figure 17
Figure 17 CBCT revealed 3-dimensionally sound implant placement No. 8; for optimum esthetic outcome, only a single implant for No. 8 was placed cantilevering pontic No. 7, avoiding central-lateral esthetic dilemma.

Figure 18
Figure 18 Patient’s smile at 1.5-year follow-up.

Figure 19
Figure 19 GALILEOS FaceScanner.

Figure 20
Figure 20 Full view at 1.5-year follow-up. (Fig 20 courtesy of Dr. Heggerick and Mr. Momma)
