Abstract
New dental cement formulations require testing to determine physical and mechanical laboratory properties. OBJECTIVES: To test an experimental calcium aluminate/glass-ionomer cement, Ceramir® C&B (CC&B), regarding compressive strength (CS), film thickness (FT), net setting time (ST) and Vickers hardness. An additional test to evaluate potential dimensional change/expansion properties of this cement was also conducted. METHODS AND MATERIALS: CS was measured according to a slightly modified ISO 9917:2003 for the CC&B specimens. The samples were not clamped while being exposed to relative humidity of >90% at 37°C for 10 minutes before being stored in phosphate-buffered saline at 37°C. For the CS, four groups were tested: Group 1—CC&B; Group 2—RelyX™ Luting Cement; Group 3—Fuji Plus™; and Group 4—RelyX™ Unicem. Samples from all groups were stored for 24 hours before testing. Only CC&B was tested for ST and FT according to ISO 9917:2003. The FT was tested 2 minutes after mixing. Vickers hardness was evaluated using the CSM Microhardness Indentation Tester using zinc phosphate cement as a comparison material. Expansion testing included evaluating potential cracks in feldspathic porcelain jacket crowns (PJCs). RESULTS: The mean and standard deviation after 24 hours were expressed in MPa: Group 1 = 160 ± 27; Group 2 = 96 ± 10; Group 3 = 138 ± 15; Group 4 = 157 ± 10. A single-factor ANOVA demonstrated statistically significant differences between the groups (P < 0.001). Pair-wise statistical comparison demonstrated a statistically significant difference between Groups 1 and 2. No statistically significant differences were found between other groups. The FT was 16.8 ± 0.9 µm and the ST was 4.8 ± 0.1 min. Vickers hardness for Ceramir C&B was 68.3 ± 17.2 and was statistically significantly higher (P < 0.05) than Fleck’s™ Zinc Phosphate cement at Vickers hardness of 51.4 ± 10. There was no evidence of cracks due to radial expansion in PJCs by the Ceramir C&B cement. CONCLUSION: All luting cements tested demonstrated compressive strengths well in excess of the ISO requirement for water-based cements of no less than 50 MPa. Ceramir C&B showed significantly higher CS than RelyX Luting Cement after 24 hours, but was not significantly higher than either Fuji Plus or RelyX Unicem. The ST and FT values of CC&B conform to and are within the boundaries of the requirements of the standard. Surface hardness was statistically higher than and comparable to zinc phosphate cement. There was no evidence of potentially clinically significant and deleterious expansion behavior by this cement. All cements tested demonstrated acceptable strength properties. Within the limits of this study, Ceramir C&B is deemed to possess physical properties suitable for a dental luting cement.
Dental luting cements perform the critical function of forming a stable interface between a fixed restoration and supporting tooth structure. Although not directly exposed to the oral environment, except in marginal areas of the restoration, dental luting cements can undergo significant stresses and effects from masticatory forces due to the nature of the environment in the oral cavity. Mechanical properties of various luting cements can differ considerably, and, hence, evaluation and documentation of these properties is necessary.1 The success of fixed restorations to a large extent depends on the type of luting agent used. Biocompatibility, insolubility, and resistance against degradation are requirements that maintain the seal at the margins of the restorations, which prevents ingress of bacteria that leads to leakage, sensitivity, and secondary decay.
Luting cements have progressed over the years through various chemistries, namely: zinc phosphate, polycarboxylate, glass ionomer, resin, resin-modified glass-ionomer (RMGI) cements, and self-adhesive resin cements. Each of these cement types or classifications possesses unique chemical characteristics, physical properties, and even, in some instances, potential therapeutic properties.2 A recently developed cement formulation consists of a hybrid calcium aluminate/glass-ionomer cement. This cement, Ceramir® C&B (CC&B) (Doxa Dental AB, www.ceramirus.com), is a new dental luting agent intended for permanent cementation of crowns and bridges, gold inlays and onlays, prefabricated metal and cast post and cores, and all-zirconia or all-alumina crowns. The cement is a water-based composition comprising calcium aluminate and glass-ionomer components, and has been demonstrated to be bioactive.3
It is well recognized that any new luting cement (or for that matter, any new dental material) should be characterized by a number of laboratory physical and mechanical tests to elucidate that material’s physical properties. Therefore, the objective of this experimental study was to test CC&B regarding net setting time, film thickness, and compressive strength according to International Organization for Standardization (ISO) 9917-1 (Water based cements – Part 1: Powder/Liquid acid-base cements).4 Three other commercially available cements were also subjected to compressive-strength testing for comparison to the test cement. Vickers surface hardness and a laboratory clinical simulation test to assess potential effects of cement dimensional change and expansion were also included in this testing. The hypothesis or experimental question posed concerned whether the calcium aluminate/glass-ionomer cement would display physical properties equal to or better than current test standards for water-based cements, and similar to current physical properties displayed by other types of luting cements.
Methods and Materials
Compressive Strength
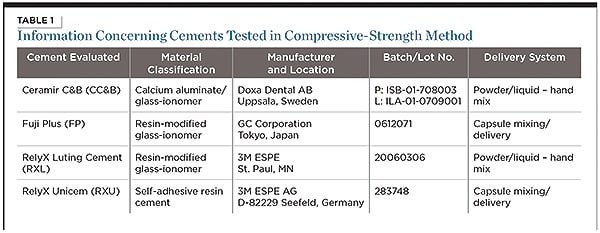
The compressive strength of CC&B luting cement was measured according to ISO 9917:1(2003), Annex D, with a minor modification (ISO 9917-1, 2003).4 (The modification was that the CC&B test material, while still in the stainless-steel mold during setting, was maintained in 100% humidity during early setting [a step not listed in the ISO test method] due to the fact that it is a hydraulic cement and sets optimally in a somewhat moist or high humidity environment during initial setting.) Information concerning the cements included in this compressive-strength testing is provided in Table 1.
Specimens 6 mm in height and 4 mm in diameter were prepared as per the sponsor’s directions for dispensing and mixing. CC&B powder and liquid were used at a liquid-to-powder ratio of 7 drops of liquid to 1 premeasured vial of powder (mass powder/liquid ratio of 3.2). Prior to opening the glass powder vial, it was lightly tapped with a metal hand instrument to ensure that the powder was free-flowing and could completely be dispensed from the vial. After mixing the powder and liquid for approximately 30 to 35 seconds (45 seconds maximum), the split cylindrical Teflon-coated stainless-steel molds were filled with the mixed cement material, covered with coated mixing pad paper, and placed in a humid environment at 37°C for 10 minutes. The mold was opened, the specimens were lightly polished to create flat uniform areas, and the specimens were placed in phosphate-buffered saline (PBS) for 24 hours. The 24-hour specimens were removed and tested in an Instron® (Model #5569) Universal Testing Machine (Instron Industrial Products, www.instron.com) with a 50-kN load cell (series 2525) under compressive load at a strain-rate of 0.75 mm/m. Control materials—RelyX™ Luting Cement (3M ESPE, www.3MESPE.com), RelyX™ Unicem Aplicap™ (3M ESPE), and Fuji Plus™ (GC America, www.gcamerica.com)—were dispensed and mixed according to the manufacturers’ recommended directions for use and allowed to set at 37°C under humid conditions for 10 minutes, lightly finished to create uniform surfaces, and stored in distilled water at 37°C for 24 hours prior to testing, under identical load and strain-rate conditions as used for the CC&B cement. Similar to other published studies evaluating compressive strength of dental cements, six specimens per test group were prepared and tested in this compressive-strength protocol.5-7 Statistical analysis of the data was accomplished via calculation of the descriptive statistics (mean values and standard deviations) for each experimental group, and statistical significance of the mean values of the data, due solely to the influence of the materials tested, was determined by a one-way ANOVA, with ranking of multiple mean values using pair-wise multiple comparisons.
Film Thickness
Film thickness of the calcium aluminate/glass-ionomer cement was measured according to the test method described in the International Standard test method (ISO 9917:1[2003], Annex C).8 The film thickness of the cement was recorded as the difference in thickness of the plates with and without the cement film, after a specified load of 150-N was applied as per this test method. The test was repeated four times, and the average of the four tests was recorded. A Mitutoyo ABS micrometer (Mitutoyo America Corporation, www.mitutoyo.com) was used to record the thickness of the plates with and without cement.
Setting Time
A 1-mm diameter cylinder was applied to the surface of the mixed cement using a 400-gram indenter applied for 5-second intervals. Setting time was determined when the cement could no longer be penetrated. The net setting time was recorded as the time elapsed between the end of mixing and the time when the needle failed to make a complete circular indentation in the cement. As per the ISO test method, the test was repeated three times.
Surface Hardness
Surface hardness of the experimental CC&B was tested using a computerized dynamic indentation tester that controlled and recorded indentation depth and force in real-time (CSM Instruments, www.csm-instruments.com). Circular specimens that were 8 mm in diameter and 4 mm thick of CC&B and a control cement—Fleck’s® Zinc Phosphate cement (Mizzy, Keystone Dental, www.keystoneind.com)—were prepared. The cement specimens were prepared as per the manufacturers’ instructions, and after setting for 10 minutes at 37°C (in 100% humidity), the surfaces of the samples were finished sequentially with 800 to 1200 silicon carbide paper on a table-top rotating polisher (Model 900, Electron Microscopy Sciences, www.electronmicroscopysciences.com) to a visual endpoint observed under a microscope at 50x magnification. CC&B and Fleck’s Zinc Phosphate specimens were incubated, respectively, in PBS and distilled water for 24 hours at 37°C. The specimens were tested in a CSM Dynamic Microhardness Tester under conditions of 0.5 newton load, 30-second load, 10-second hold, and 30-second unload loading cycle. A Poisson’s ratio of 0.34 was used to calculate the microhardness of the samples. Statistical analysis of the data (n = 7) was accomplished via calculation of the descriptive statistics (mean values and standard deviations) for each experimental group, and statistical significance of the data was determined by a one-way ANOVA.
Sequelae of Expansion—Cementation of Porcelain Jacket Crowns
As per a modification of a technique reported by Leevailoj et al,9 the tooth preparation was a standard, 360-degree shoulder finish-line preparation, with uniform reduction. Porcelain jacket crowns (PJCs) were cemented with CC&B (n = 10) or Fuji Plus (n = 5) and stored in an incubator in PBS at 37°C and examined over extended time periods (3 years) for external cracks and/or craze lines in the ceramic material. Tooth types selected for this test included maxillary incisors, cuspids, and premolars. Porcelain crown thickness reflected the anatomical contour of the teeth to replace tooth structure removed by a standard porcelain jacket crown preparation. This test method serves as an indirect measure to access development of internal expansion stresses to induce possible vertical fractures due to cement expansion stress. Low-strength, feldspathic porcelain (Ceramco® II, DENTSPLY, www.dentsply.com) was used as the ceramic material. Each cemented crown was examined every 2 to 3 days for 1 month by a microscope under illumination with an LED light at 10x magnification to assess for vertical or horizontal crack formation. At the end of 30 days, crowns were examined weekly for up to 52 weeks. Subsequently, periodic examinations were made over the following 2 years. Data were presented as the number of crowns (out of a total of 10 crowns for the experimental cement and five for the control cement) with evidence of cracks or fractures as a function of time of immersion.
Results
Compressive Strength
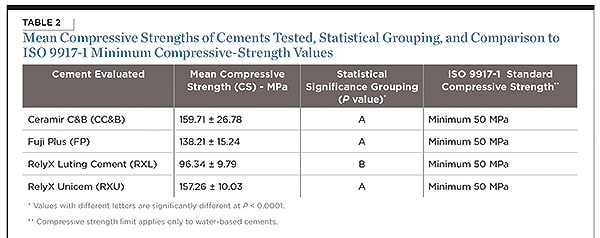
The data and results of the compressive strength testing in this study are listed in Table 2.
One-way ANOVA indicated a statistically significant difference in 24-hour compressive strengths affected by the type of material tested (P < 0.001). Pair-wise statistical analysis of the data in Table 2 comparing CC&B to RelyX Luting Cement (a RMGI cement) indicated statistically significant difference between the mean values of these groups (P < 0.001). However, pair-wise statistical analysis indicated no statistically significant difference in 24-hour compressive strengths (P < 0.05) comparing CC&B to RelyX Unicem (a self-etching, resin cement; P = 0.838). Likewise, pair-wise statistical analysis of the above data indicated no statistically significant difference in 24-hour compressive strengths (P < 0.05) comparing CC&B to Fuji Plus (a RMGI cement; P = 0.118).
Setting Time Assessment
Assessment of setting time was conducted as per the ISO Standard 9917-1 (2003) for the determination of cement setting time. Acceptable setting time was determined by applying the acceptable range of setting times for a glass-ionomer cement, as described: minimum (glass-ionomer luting) = 1.5 minutes; maximum (glass-ionomer luting) = 8.0 minutes. A series of three separate setting-time measurements was taken for three separate mixes of the CC&B cement. The data were as follows: 4 minutes, 45 seconds; 4 minutes, 50 seconds; and 4 minutes, 50 seconds. The average setting time was thus determined to be 4.8 ± 0.1 min.
Film Thickness
The assessment of film thickness for CC&B arrived at an overall average value of 16.4 (0.89) µm.
The values for film thickness and setting time are depicted in Table 3.
Surface Hardness
The Vickers hardness value for CC&B was 68.3 ± 17.2. The Vickers hardness value for the comparative cement, zinc phosphate, was 51.4 ± 10. A statistically significant difference between these values was established (P = 0.043).
Sequelae of Expansion—Cementation of Porcelain Jacket Crowns
There was no evidence of any fractures occurring in any of the 10 porcelain jacket crowns cemented with CC&B over the 3-year observation period. The same was observed for the control cement, Fuji Plus; all five (5) porcelain crowns were intact. The cemented PJCs on the prepared extracted teeth are photographically represented in Figure 1.
Discussion
The results of the compressive-strength testing clearly demonstrate that both RMGI materials (RelyX Luting Cement [RXL] and Fuji Plus [FP]), the self-adhesive resin cement (RelyX Unicem [RXU]), and the calcium aluminate/glass-ionomer cement (Ceramir C&B [CC&B]) all exceeded the required strength level set by ISO Standard 9917-1. CC&B performed acceptably and clearly met the Standard’s compressive-strength requirement, with a mean 24-hour compressive strength that exceeded the minimum required compressive strength under the Standard (50 MPa) by more than a factor of 3. CC&B’s mean 24-hour compressive-strength value of approximately 160 MPa was comparable to the mean compressive strength of a well-established self-adhesive resin cement, RelyX Unicem, at a mean compressive strength of approximately 157 MPa. CC&B was statistically stronger in its mean 24-hour compressive strength than one of the two RMGIs tested in this study, RelyX Luting Cement. It should be noted that the results of this study are comparable to values determined in other published studies of the mechanical-strength properties of luting cements. For example, the authors’ value for the compressive strength of RelyX Luting Cement (formerly Vitremer Luting Cement) of approximately 90 MPa to 100 MPa is similar to that of Piwowarczyk and Lauer10 and Li and White.11 Kumbuloglu et al12 reported a mean compressive strength value of approximately 145 MPa for RelyX Unicem Aplicap, which also compares very favorably to the value obtained in this study for that material. In the first published report of strength properties of a calcium aluminate cement for dental use, Lööf et al13 reported mean compressive-strength values in a similar range to those documented in this report for the hybrid calcium aluminate/glass-ionomer material.
Alternative test methods, such as flexural strength, have been recommended and used for strength testing for luting cements, especially if their composition contains resin components. This alternative test methodology is used in the ISO Standard 9917 – Part 2. The compressive strength method used here was adopted due to the fact that the test cement being evaluated in this study, and most of the cements recognized as bioactive or potentially bioactive, are water-based. The literature, as documented in this paper’s cited references, also suggests that this compressive-strength protocol has been and continues to be used for a wide range of cement chemistries for comparative purposes.
It is intuitively obvious to any clinician that film thickness is a critical parameter for any permanent dental luting cement. The inclusion of a test for film thickness in the ISO Standard further amplifies this fact. Using the prescribed testing methodology of ISO 9917-1, the film thickness of CC&B was determined to meet the standard with a film thickness of less than 25 µm. As per the ISO 9917-1 requirement, a set of five measures were taken, which resulted in all five film thickness measures at or below 17 µm, with an average value of 16.4 (0.89), a value well within the guidelines of the ISO standard for luting cement film thickness.
While the viscosity of this cement was not measured directly, the handling and consistency of the cement during seating of restorations suggests a viscosity behavior consistent with Newtonian flow properties with a lack of pseudo plastic flow characteristics that could impede complete seating of restorations.
Setting time is defined as the period of time measured from the end of mixing until the material has set according to the criteria and conditions specified in Annex A, International Standard, ISO 9917:1. Setting time is an important clinical property for a luting cement. As per the Standard’s test method, all of the setting times of the three cement mixes were well within the net setting time standard (minimum/maximum setting times) of 2.5/8.0 minutes for zinc phosphate cement, and 1.5/6.0 minutes for glass polyalkenoate cements. The average value of these setting times was 4.8 ± 0.1 minutes. CC&B met the setting time prescribed by the applicable International Standard.
Surface hardness relates to the ability of a material to resist permanent deformation, usually measured in some form of an indentation model. Nevertheless, one formal text in the subject of dental materials14 also suggests that “hardness is indication of … resistance to in-service scratching.” Jastrzebski amplifies this property stating that: “The hardness of a material can be measured by its resistance to scratching or to indentation.”15 Although a relationship between surface hardness and abrasion resistance in a dental cement is not directly proportional,16 it should be noted that in one investigation, such a relationship did in fact exist between the materials exhibiting the relative highest/lowest values in terms of surface hardness and abrasion resistance for a group of glass-ionomer materials.16 In another study, which compared the toothbrush-dentifrice abrasion of RMGIs, there did appear to be a proportional relationship between abrasion resistance and surface hardness for the three RMGIs evaluated.17 In fact, these authors concluded: “The lower abrasion resistance found in the resin-modified products appears to be related to their lower surface hardness.” The comparative-reference material used in this test, zinc phosphate cement, has a long and established successful clinical history as a dental luting cement. CC&B demonstrated a mean Vickers hardness quite comparable to that measured for zinc phosphate cement, suggesting that this new cement has a resistance to permanent deformation—which may be a component in the process of surface scratching or application of certain abrasives—similar to that of the well established zinc phosphate cement.
Using a method described previously by Leevailoj et al,9 the cementation of PJC restorations to extracted teeth with the experimental cement represents an alternative method to assess whether any luting cement produces dimensional changes and resultant lateral forces sufficient to cause iatrogenic damage or cracks in weak full-coverage ceramic restorations. Those authors reported the ability to differentiate a potentially adverse effect among various types of cements used in this specific cementation procedure. The results of this approach applied in this study using the calcium aluminate/glass-ionomer cement clearly demonstrate an absence of any damage to these feldspathic porcelain-based crowns for up to a 2-year observation period, with the latter material being one that has an inherently low tolerance to tensile forces of a low magnitude, as would be generated by internal expansion or lateral “hoop” stresses.
The PJC test was conducted, in part, as a result of prior reports suggesting that calcium aluminate cements may undergo water sorption and dimensional change levels sufficient to produce lateral tangential forces sufficient to damage or crack natural tooth structure.18,19
The fact that this previously studied calcium aluminate cement lacked any polymerizable resin components, especially hydrophilic resin monomers that could act as water-adsorbing hydrogels, made the mechanism for this hypothesized behavior unclear. Nevertheless, the results found using the test method employed in this study to analyze potential expansion by this new cement over an observation period of up to 2 years indicated that CC&B did not produce, in a clinically modeled test method, potentially damaging expansion forces.
The findings of this study suggest that a new calcium aluminate/glass-ionomer cement possesses physical properties comparable to other currently used luting cements. Still, one might inquire about how the physical properties and performance behavior of this particular bioactive dental cement compare to other bioactive cement chemistries. The earliest of the bioactive cement formulations proposed for dental restorative purposes, the self-setting calcium phosphate cements, first appeared in the late 1980s.20 While highly biocompatible and displaying the ability to form hydroxyapatite under appropriate solution conditions, the compressive strengths of these first bioactive cement formulas were low (compared to other dental cements) and on the order of 30 MPa to 40 MPa.21 Another class of bioactive cements, the calcium silicates, are available commercially as a well known root-end filling/pulp capping/root replacement material, mineral trioxide aggregate (MTA).22 MTA has been shown to be bioactive23 but its documented 24-hour compressive strength of 40 MPa positions it as initially weaker than other dental cements such as Super-EBA or IRM.24
Two specific approaches to incorporate bioactivity (ie, apatite forming capability) into glass-ionomer cements have also been documented in the literature. One avenue has been the incorporation of particles of bioactive glass into a glass-ionomer cement.7 Unfortunately, increasing proportions of bioactive glass particles into the glass-ionomer reduced the cement’s compressive strength from a baseline mean level of 120 MPa to 100 MPa or less. Similarly, the surface hardness of these experimental cements was also reduced by these modifications. Another strategy explored with glass-ionomer cements—again, to improve their remineralization potential—has been the incorporation of incremental amounts of a calcium-based remineralizing agent, casein phosphopeptide-amorphous calcium phosphate (CCP-ACP).25 It is interesting to note that the incorporation of 1.56% w/w CCP-ACP into the powder of a commercially available glass-ionomer restorative (Fuji IX, GC Corporation) significantly increased the compressive strength of this glass-ionomer material, raising the compressive strength of the control material from a mean of 138 MPa to 170 MPa. In reviewing the spectrum of bioactive or remineralizing cements that have been studied thus far and cited above, the strength characteristics of the calcium aluminate/glass-ionomer cement presented in this paper appear encouraging and merit further exploration in the realm of dental materials for restorative purposes.
Conclusions
As a result of this study, the authors conclude the following:
• All cements tested demonstrated mean compressive-strength values in considerable excess of the ISO 9917-1 Standard minimum value of 50 MPa.
• The calcium aluminate/glass-ionomer cement (CC&B) showed significantly higher compressive strength than one of the resin-modified glass-ionomer (RMGI) cements (RXL) after 24 hours and a mean compressive strength comparable to the other RMGI (FP) and the self-adhesive resin cement (RXU).
• The net setting time of the CC&B calcium aluminate/glass-ionomer cement (4.8 m) is within the requirement of ISO 9917-1.
• The film thickness of the CC&B calcium aluminate/glass-ionomer cement (16.8 µm) conformed to the ISO 9917-1 requirement of 25 µm.
• The CC&B calcium aluminate/glass-ionomer cement does not appear to exert deleterious expansive pressure effects of clinical consequence, based on laboratory tests of porcelain jacket crowns.
• Within the limits of this study, Ceramir® C&B and the luting cements to which it was compared—RelyX Luting, RelyX Unicem, and Fuji Plus—all appear to meet the compressive-strength requirements described in ISO 9917-1 (2003) for a water-based dental luting cement.
DISCLOSURE
This study was supported in part by Doxa Dental AB, Uppsala, Sweden.
ABOUT THE AUTHORS
Steven Jefferies, DDS, PhD
Professor, Department of Restorative Dentistry, Kornberg School of Dentistry, Temple University, Philadelphia, Pennsylvania
Jesper Lööf, PhD
Director of Research, Doxa Dental AB, Uppsala, Sweden
Cornelis H. Pameijer, DMD, MScD, DSc, PhD
Professor Emeritus, University of Connecticut, Farmington, Connecticut
Daniel Boston, DMD
Associate Professor and Chairman, Department of Restorative Dentistry, Kornberg School of Dentistry, Temple University, Philadelphia, Pennsylvania
Colin Galbraith, DMD
Resident, Oral and Maxillofacial Surgery, Denver Health Medical Center, Denver, Colorado
Leif Hermansson, AB, PhD
Chief Scientific Advisor, Founder, and Director, Doxa Dental AB, Uppsala, Sweden
REFERENCES
1. Hondrum SO. Storage stability of dental luting cements. J Prosthet Dent. 1999;81(4):464-468.
2. Attar N, Tam LE, McComb D. Mechanical and physical properties of contemporary dental luting agents. J Prosthet Dent. 2003;89(2):127-134.
3. Lööf J, Svahn F, Jarmar T, et al. A comparative study of the bioactivity of three materials for dental applications. Dent Mater. 2008;24(5):653-659.
4. International Organization for Standardization. Dentistry—Water-based cements—Part 1: Powder/liquid acid-base cements. Geneva, Switzerland; 2007. ISO 9917-1:2003.
5. Mitra SB, Kedrowski BL. Long-term mechanical properties of glass ionomers. Dent Mater. 1994;10(2):78-82.
6. Prentice LH, Tyas MJ, Burrow MF. The effect of mixing time on the handling and compressive strength of an encapsulated glass-ionomer cement. Dent Mater. 2005;21(8):704-708.
7. Yli-Urpo H, Lassila LV, Närhi T, Vallittu PK. Compressive strength and surface characterization of glass ionomer cements modified by particles of bioactive glass. Dent Mater. 2005;21(3):201-209.
8. International Organization for Standardization. Dentistry—Water-based cements—Part 1: Powder/liquid acid-base cements, Annex C—Determination of film thickness (luting cements only). Geneva, Switzerland; 2007. ISO 9917-1:2003.
9. Leevailoj C, Platt JA, Cochran MA, Moore BK. In vitro study of fracture incidence and compressive fracture load of all-ceramic crowns cemented with resin-modified glass ionomer and other luting agents. J Prosthet Dent. 1998;80(6):699-707.
10. Piwowarczyk A, Lauer HC. Mechanical properties of luting cements after water storage. Oper Dent. 2003;28(5):535-542.
11. Li ZC, White SN. Mechanical properties of dental luting cements. J Prosthet Dent. 1999;81(5):597-609.
12. Kumbuloglu O, Lassila LV, User A, Vallittu PK. A study of the physical and chemical properties of four resin composite luting cements. Int J Prosthodont. 2004;17(3):357-363.
13. Lööf J, Engqvist H, Ahnfelt NO, et al. Mechanical properties of a permanent dental restorative material based on calcium aluminate. J Mater Sci Mater Med. 2003;14(12):1033-1037.
14. Sakaguchi RL, Powers JM. Mechanical properties. In: Sakaguchi RL, Powers JM, eds. Craig’s Restorative Dental Materials. 12th ed. St. Louis, MO: Mosby; 2006:79.
15. Jastrzebski ZD. Strength and fracture. In: Jastrzebski ZD, ed. The Nature and Properties of Engineering Materials. 2nd ed. New York, NY: John Wiley & Sons, Inc; 1976:263-265.
16. Forss H, Seppä L, Lappalainen R. In vitro abrasion resistance and hardness of glass-ionomer cements. Dent Mater. 1991;7(1):36-39.
17. Momoi Y, Hirosaki K, Kohno A, McCabe JF. In vitro toothbrush-dentifrice abrasion of resin-modified glass ionomers. Dent Mater. 1997;13(2):82-88.
18. Sunnegårdh-Grönberg K, van Dijken JW, Lindberg A, Hörstedt P. Interfacial adaptation of a calcium aluminate cement used in class II cavities, in vivo. Clin Oral Invest. 2004;8(2):75-80.
19. Berglund A, Hulterström AK, Gruffman E, van Dijken JW. Dimensional change of a calcium aluminate cement for posterior restorations in aqueous and dry media. Dent Mater. 2006;22(5):470-476.
20. Brown WE, Chow LC, inventors; American Dental Association Health Foundation, assignee. Dental restorative cement pastes. US Patent 4 518 430. May 21, 1985.
21. Fukase Y, Eanes ED, Takagi S, et al. Setting reactions and compressive strengths of calcium phosphate cements. J Dent Res. 1990;69(12):1852-1856.
22. Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review—Part 1: chemical, physical, and antibacterial properties. J Endod. 2010;36(1):16-27.
23. Gandolfi MG, Taddei P, Tinti A, Prati C. Apatite-forming ability (bioactivity) of ProRoot MTA. Int Endod J. 2010;43(10):917-929.
24. Torabinejad M, Hong CU, McDonald F, Pitt Ford TR. Physical and chemical properties of a new root-end filling material. J Endod. 1995;21(7):349-353.
25. Mazzaoui SA, Burrow MF, Tyas MJ, et al. Incorporation of casein phosphopeptide-amorphous calcium phosphate into a glass-ionomer cement. J Dent Res. 2003;82(11):914-918.