Abstract
OBJECTIVE: To determine the effectiveness of a water flosser in reducing the bleeding on probing (BOP) index around dental implants as compared to flossing. METHODS AND MATERIALS: Patients with implants were randomly assigned to one of two groups in this examiner-masked, single-center study. The study compared the efficacy of a manual toothbrush paired with either traditional string floss or a water flosser. RESULTS: The primary outcome was the reduction in the incidence of BOP after 30 days. There were no differences in the percent of bleeding sites between the groups at baseline. At 30 days, 18 of the 22 (81.8%) implants in the water flosser group showed a reduction in BOP compared to 6 of the 18 (33.3%) in the floss group (P = 0.0018). CONCLUSIONS: These results demonstrate that the water flosser group had statistically significantly greater bleeding reduction than the string floss group. The authors concluded that water flossing may be a useful adjuvant for implant hygiene maintenance.
Peri-implant mucositis is an inflammatory lesion of the mucosa surrounding an implant. Its pathogenesis and visual appearance is similar to gingivitis.1 If there is evidence of bone loss (peri-implantitis), the implant is at increased risk for failure. Peri-implantitis is similar to periodontitis clinically but differs histopathologically.2 Peri-implant mucositis occurs in approximately 80% of individuals who have implants or about 50% of implant sites, and peri-implantitis occurs in 28% to 56% of people with implants or 12% to 40% of implant sites.3
The subgingival microbiota is a mix of anaerobic bacteria dominated by Gram-negative organisms similar to chronic periodontal infections.4 Bleeding is a standard measure used to diagnose mucositis. The absence of bleeding is generally indicative of peri-implant stability.5,6
Poor plaque control is one of the risk factors for the initiation and proliferation of peri-implant diseases.7 The goal of oral hygiene with implants is to reduce the biofilm and subsequent infection. Due to clinical similarities, home care recommendations tend to mimic those for dentate individuals such as brushing, flossing, and rinsing. A recent systematic review reported there is no reliable evidence demonstrating an effective intervention for treating peri-implant disease.8 Clearly there is a need for studies that measure the success and safety of different methods and devices for daily cleansing around implants and prosthetic replacements. The objective of this study was to determine the efficacy of a water flosser in reducing bleeding on probing (BOP) index around dental implants as compared to traditional string floss.
Methods and Materials
Subjects
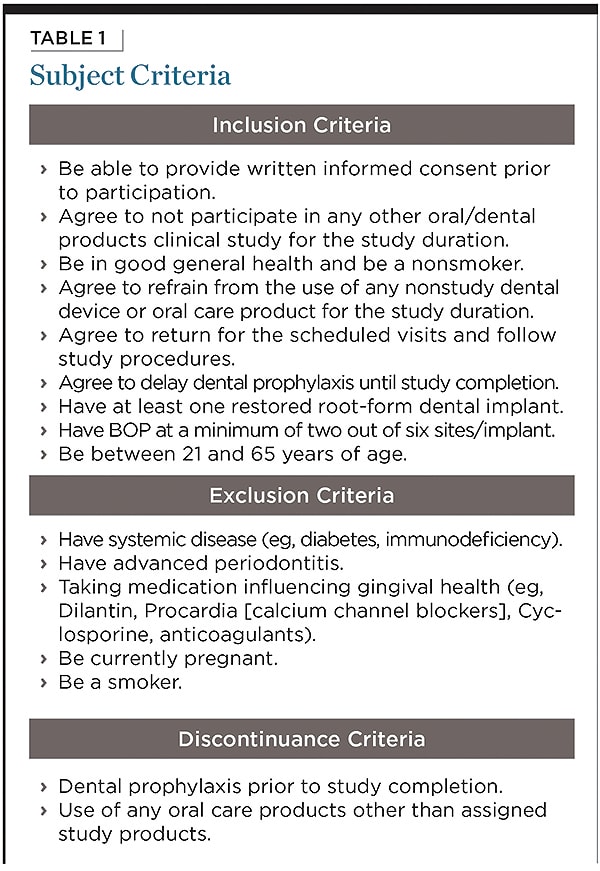
Adult subjects between 22 and 62 years of age were recruited from the Boston, Massachusetts area. Exclusion and inclusion criteria were assessed (Table 1). To qualify, a subject must have had at least two out of six sites of bleeding on probing present on at least one implant. If a subject had more than one implant that qualified, up to two implants were included in the study.
If a subject had more than two implants that qualified for the study, two of the implants were chosen for inclusion in the study using a computer-generated randomization scheme.
The study forms and protocol were approved by the Institutional Review Board at Tufts Medical Center and Tufts University Health Sciences Campus. Subjects read and signed the informed consent and received a copy for their records at the screening/baseline visit.
Study Design
This university-based (Tufts University School of Dental Medicine), examiner-blind, double-arm, parallel-group, single-center study compared the efficacy of a manual toothbrush paired with either traditional string floss or a water flosser. The entire study lasted 4 months, including a 3-month recruitment period and a 1-month evaluation period. The subjects were randomized to one of two groups by way of a computer-generated randomization scheme. Randomization was performed at the subject level and not the implant level, resulting in 22 implants in each group. The allocation ratio was 1:1. A spreadsheet generated by the statistician and viewed by the research coordinator (and not the examiners) at the time a subject was enrolled contained the randomization scheme. A research coordinator also enrolled participants and assigned them to the randomized group. Examiners were blinded to the subject’s treatment group.
Demographic data and medical history were collected. Subjects received a comprehensive oral examination to evaluate the oral and perioral region, including hard and soft tissues. All subjects used an American Dental Association (ADA) standard manual toothbrush (Oral-B® Soft Compact 35, Procter & Gamble, www.pg.com) and an ADA-standard dentifrice (Crest® Cavity Protection Gel Toothpaste, Procter & Gamble).
Group 1 (String Floss [SF]) was assigned unflavored waxed string floss, and Group 2 (Water Floss [WF]) was assigned a water flosser and specialized tip. Test products were distributed away from the examiner. Subjects were given tooth brushing instructions for the Bass technique. The SF group received standard flossing instructions, and the WF group received manufacturer’s instructions. Subjects used all of their products under the direction of the research coordinator before being allowed to take them home, and they were given written instructions to follow at home and a log in which to track brushing and flossing or water flossing. Subjects in both groups were instructed to brush twice a day (morning and evening) for 2 minutes each time using a sand timer. Subjects in the SF group flossed before brushing in the evening. Subjects in the WF group used the water flosser and specialized tip at pressure setting number 6 (medium) with 500 ml of lukewarm water before brushing in the evening. All subjects refrained from using any other oral hygiene aid or agent during the study.
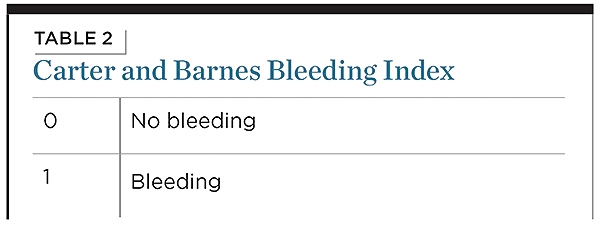
A trained examiner recorded BOP at six sites per implant (ie, mesio-facial, facial, disto-facial, mesio-lingual, lingual, and disto-lingual) using a plastic probe at screening/baseline, day 14, and day 30 (Table 2).
At visit 2 (Day 14) and visit 3 (Day 30), discontinuance criteria were assessed (Table 1). Subjects received a comprehensive oral examination and the bleeding index was recorded at six sites per implant. Subjects brought the tooth brushing log to this visit, and the log was checked to ensure that the subject was complying with instructions.
Study Products
The water flosser (Waterpik® Ultra Water Flosser, Water Pik, Inc., www.waterpik.com) is a pulsating device that delivers water or other solution to clean interdentally and subgingivally. The device has a reservoir for the solution, variable pressure control, and a handle for tip placement (Figure 1). Subjects used a specialized tip (Plaque Seeker® Tip, Water Pik, Inc.) designed with an orifice to deliver the irrigant surrounded by three individual tufts of soft nylon bristles (Figure 2). The tip is directed at the gingival margin and interdental areas of the prostheses attached to the implant from the lingual and buccal area.
Unflavored waxed string dental floss (Reach®, Johnson & Johnson Oral Care Company, www.jnj.com) was provided to the subjects in the SF group. Subjects cleaned the proximal surfaces of the implants following instruction for wrapping the floss on the mesial and distal surfaces of the prosthesis forming a “C” and moving the floss up and down the surface several times.
Statistical Analysis
The primary outcome measure for the study was reduction in incidence of bleeding on probing at 30 days. It was anticipated that at least 50% of the individuals in the water floss group would have bleeding at no more than one site/implant by 30 days, compared to only 10% of the individuals in the string floss group. As a result, a sample size of 20 per group would provide 80% power to detect a difference between a 50% reduction in incidence of BOP in the Waterpik group and a 10% reduction in the control group, using an exact test of two proportions, assuming alpha = 0.05 (nQuery Advisor, 7.0).
An intent-to-treat analysis was performed. Mean age at baseline was compared between the two groups using a two-sample t-test. Any P value < 0.05 was considered statistically significant. All analyses were performed using SAS® Version 9.2 (SAS Institute Inc., www.sas.com).
Results
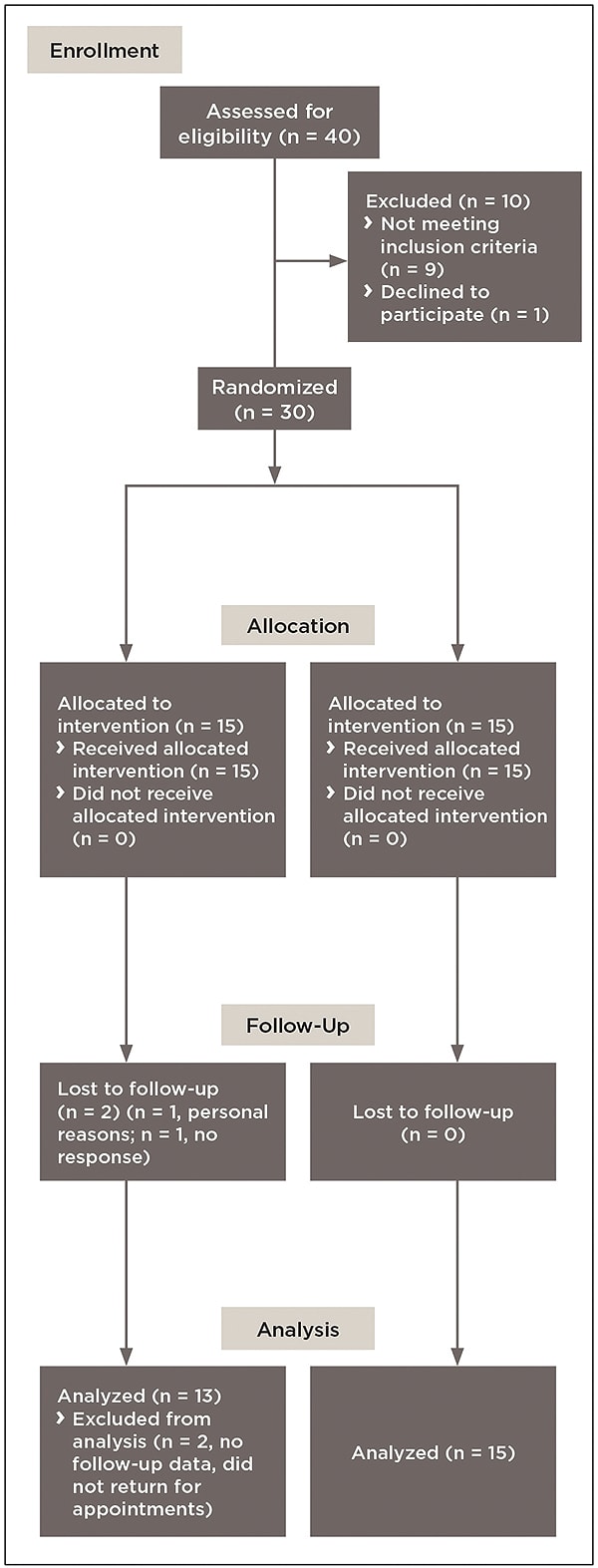
Among 40 subjects screened for the study, 30 qualified. They were entered into a randomization scheme and contributed a total of 44 implants. Two subjects completed only their baseline visit and then dropped out: one subject withdrew from the study due to personal issues that would preclude completion of the study visits; and one subject was withdrawn after repeated attempts to set up recall appointments with this individual were unsuccessful. These two subjects, both of whom were in the SF group, had contributed a total of four implants (two each). Thus, the final analysis is based on 40 implants placed in 28 subjects (Figure 3).
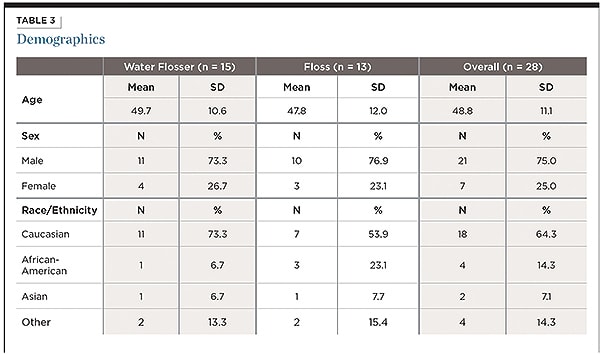
The mean (SD) age of the 15 subjects in the water flosser group was 49.7 (10.6) years; it was 47.8 (12.0) years in the 13-subject string floss group (Table 3). This difference was not statistically significant (P = 0.6730).
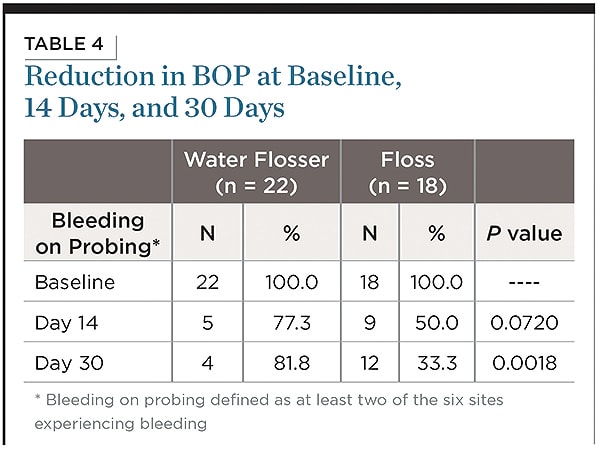
The primary outcome measure was the reduction in the incidence of bleeding on probing (BOP) after 30 days. BOP was defined as at least two of the six sites experiencing bleeding. All subjects (100%) had BOP at baseline. The percent of bleeding sites was comparable between the two groups. The mean (SD) percent of bleeding sites in the WF group was 47.0% (13.3%) and in the SF group was 52.8% (19.2%). This difference was not statistically significant (P = 0.2655). At 30 days, 18 of the 22 (81.8%) implants in the WF group experienced a reduction in BOP, compared to 6 of the 18 (33.3%) seen in the SF group. This 2.45-fold difference (145%) was highly statistically significant (P = 0.0018), suggesting an improvement in BOP for the subjects in the WF group (Table 4). No adverse events were reported during the study.
Discussion
This study evaluated the efficacy of water irrigation used with a specialized tip on the incidence of bleeding around implants. The results showed that a water flosser on medium pressure with tap water is a more effective way to reduce bleeding around implants than string floss. The results from this study are similar to findings from studies that compared water flossing to string floss on natural teeth. Barnes et al demonstrated a 40% to 93% reduction in bleeding and 51% to 53% reduction in gingivitis using a water flosser on medium pressure with only water once daily compared to string floss used once daily.9 Similarly, Rosema et al found the water flosser was significantly more effective at reducing bleeding compared to string floss with a standard tip (13% vs. 26%) and a specialized tip (13% vs. 20%). At 4 weeks, the flossing group returned to baseline measures, while the water flosser groups continued to show a significant reduction in bleeding (15% to 17%).10 A third study measured the reduction of bleeding with 11- to-17-year-olds with fixed orthodontic appliances and found a 26% better reduction in bleeding for the group using the water flosser with the orthodontic tip compared to string floss at 4 weeks.11
The number of implants placed by dentists and dental specialists is increasing based on a predictable outcome of success.12,13 A comprehensive treatment plan includes advising the patient of the risk of failure based on smoking, history of radiotherapy, and local bone quality and quantity. Peri-implant disease is a sequelea of poor oral hygiene, placement of a noncleansable prosthetic, or recommendations that are not effective for implants. Thus, one of the key factors to implant success is the adherence to an effective maintenance program.
The evidence for cleaning around implants and the prosthetic replacement is limited. A systematic review included five studies that evaluated the efficacy of an implant maintenance regimen.8 Two of the studies evaluated the efficacy of a powered toothbrush and a sonic toothbrush, with neither showing a statistically significant difference compared to manual brushing. Another study compared rinsing with an antiseptic for 30 seconds twice a day to rinsing with a placebo and reported improvements in plaque, bleeding, and gingival index compared to placebo. There were no differences in probing depth or attachment levels.
A study that compared rinsing with chlorhexidine to irrigating with a subgingival delivery tip showed a benefit in favor of the irrigation, which was found to be significantly more effective in reducing the plaque, gingivitis, and stain index over 3 months.14
This study provides clinical information on the efficacy of a water flosser on BOP around implants. Studies on natural teeth have found similar results along with the reduction of gingivitis,9,10 probing pocket depth,15 subgingival bacteria,16-18 and proinflammatory mediators as measured in the gingival crevicular fluid or blood serum.15,19 The ability to access20,21 and remove pathogenic bacteria from pockets up to 6 mm16-18 is a benefit for implant-supported prostheses, with the best clinical outcome of 3 mm to 5 mm pockets. Water flossing has also been tested on people with orthodontics,11,22 diabetes,19 and those in periodontal maintenance.23,24
This study evaluated the efficacy of a water flosser on single implants restored with a crown. Additional studies with implant-supported dentures, bridges, and other prosthetic appliances are needed.
Conclusion
This 30-day randomized clinical trial demonstrated that a water flosser paired with a manual toothbrush is 2.45-fold (145%) more effective at reducing bleeding around implants than string floss with no adverse events reported in either group.
ACKNOWLEDGMENT
The authors would like to thank Jacob Silberstein for his assistance and support during the study.
DISCLOSURE
This study was sponsored in part by Water Pik, Inc.
ABOUT THE AUTHORS
Britta Magnuson, DMD
Instructor, Tufts University School of Dental Medicine,
Boston, Massachusetts
Masly Harsono, DMD, MS
Assistant Professor, Tufts University School of Dental Medicine, Boston, Massachusetts
Paul C. Stark, MS, ScD
Professor, Director of Advanced and Graduate Education,
Tufts University School of Dental Medicine, Boston, Massachusetts
Deborah Lyle, RDH, MS
Director of Research, Water Pik, Inc., Fort Collins, Colorado
Gerard Kugel, DMD, MS, PhD
Professor, Associate Dean for Research, Tufts University School of Dental Medicine, Boston, Massachusetts
Ronald Perry, DMD, MS
Professor, Director of the Gavel Center for Restorative Research, Tufts University School of Dental Medicine, Boston, Massachusetts
REFERENCES
1. Lang NP, Bosshardt DD, Lulic M. Do mucositis lesions around implants differ from gingivitis lesions around teeth? J Clin Periodontol. 2011;38(11 suppl):182-187.
2. Berglundh T, Zitzmann NU, Donati M. Are peri-implantitis lesions different from periodontitis lesions? J Clin Periodontol. 2011;38(11 suppl):188-202.
3. Lindhe J, Meyle J; Group D of European Workshop on Periodontology. Peri-implant diseases: Consensus Report of the Sixth European Workshop on Periodontology. J Clin Periodontol. 2008;35(8 suppl):282-285.
4. Mombelli A. Décaillet F. The characteristics of biofilms in peri-implant disease. J Clin Periodontol. 2011;38(11 suppl):203-213.
5. Jepsen S, Rühling A, Jepsen K, et al. Progressive peri-implantitis. Incidence and prediction of peri-implant attachment loss. Clin Oral Implants Res. 1996;7(2):133-142.
6. Luterbacher S, Mayfield L, Brägger U, Lang NP. Diagnostic characteristics of clinical and microbiological tests for monitoring periodontal and peri-implant mucosal tissue conditions during supportive periodontal therapy (SPT). Clin Oral Implants Res. 2000;11(6):521-529.
7. American Academy of Periodontology. Peri-implant mucositis and peri-implantitis: a current understanding of their diagnoses and clinical implications. J Periodontol. 2013;84(4):436-443.
8. Esposito M, Grusovin MG, Worthington HV. Treatment of peri-implantitis: what interventions are effective? A Cochrane systematic review. Eur J Oral Implantol. 2012;5(suppl):S21-S41.
9. Barnes CM, Russell CM, Reinhardt RA, et al. Comparison of irrigation to floss as an adjunct to tooth brushing: effect on bleeding, gingivitis, and supragingival plaque. J Clin Dent. 2005;16(3):71-77.
10. Rosema NA, Hennequin-Hoenderdos NL, Berchier CE, et al. The effect of different interdental cleaning devices on gingival bleeding. J Int Acad Periodontol. 2011;13(1):2-10.
11. Sharma NC, Lyle DM, Qaqish JG, et al. Effect of a dental water jet with orthodontic tip on plaque and bleeding in adolescent patients with fixed orthodontic appliances. Am J Orthod Dentofacial Orthop. 2008;133(4):565-571.
12. Roos-Jansåker AM, Lindahl C, Renvert H, Renvert S. Nine- to fourteen-year follow-up of implant treatment. Part I: implant loss and associations to various factors. J Clin Periodontol. 2006;33(4):283-289.
13. Nixon KC, Chen ST, Ivanovski S. A retrospective analysis of 1,000 consecutively placed implants in private practice. Aust Dent J. 2009;54(2):123-129.
14. Felo A, Shibly O, Ciancio, et al. Effects of subgingival chlorhexidine irrigation on peri-implant maintenance. Am J Dent. 1997;10(2):107-110.
15. Cutler CW, Stanford TW, Abraham C, et al. Clinical benefits of oral irrigation for periodontitis are related to reduction of pro-inflammatory cytokine levels and plaque. J Clin Periodontol. 2000;27(2):134-143.
16. Cobb CM, Rodgers RL, Killoy WJ. Ultrastructural examination of human periodontal pockets following the use of an oral irrigation device in vivo. J Periodontol. 1988;59(3):155-163.
17. Drisko CL, White CL, Killoy WJ, Mayberry WE. Comparison of dark-field microscopy and a flagella stain for monitoring the effect of a Water Pik on bacterial motility. J Periodontol. 1987;58(6):381-386.
18. Chaves ES, Kornman KS, Manwell MA, et al. Mechanism of irrigation effects on gingivitis. J Periodontol. 1994;65(11):1016-1021.
19. Al-Mubarak S, Ciancio S, Aljada A, et al. Comparative evaluation of adjunctive oral irrigation in diabetics. J Clin Periodontol. 2002;29(4):295-300.
20. Braun RE, Ciancio SG. Subgingival delivery by an oral irrigation device. J Periodontol. 1992;63(5):469-472.
21. Eakle WS, Ford C, Boyd RL. Depth of penetration in periodontal pockets by oral irrigation. J Clin Periodontol. 1986;13(1):39-44.
22. Burch JG, Lanese R, Ngan P. A two-month study of the effects of oral irrigation and automatic toothbrush use in an adult orthodontic population with fixed appliances. Am J Orthod Dentofacial Orthop. 1994;106(2):121-126.
23. Newman MG, Cattabriga M, Etienne D, et al. Effectiveness of adjunctive irrigation in early periodontitis: multi-center evaluation. J Periodontol. 1994;65(3):224-229.
24. Flemmig TF, Epp B, Funkenhauser Z, et al. Adjunctive supragingival irrigation with acetylsalicylic acid in periodontal supportive therapy. J Clin Periodontol. 1995;22(6):427-433.