Abstract
Implant placement has continued to gain acceptance as a viable solution for the treatment of missing teeth, serving as an alternative to dentures or bridges. However, clinicians must be aware of and capable of handling complications that may accompany the placement of dental implants. Complications can range from prosthetic problems stemming from misalignment of implants, to fixed/removable prosthesis-related complications, to screw-connection impediments. This article describes and illustrates how a multidisciplinary team approach can be employed to optimize implant treatment planning to successfully overcome these issues.
It is essential that implant therapy be guided by a multidisciplinary team that first determines the functional, esthetic, and long-term maintenance requirements of a final prosthesis. Utilizing that information, the team can access the surgical requirements and limitations critical to support the prosthesis. If needed surgical procedures are deemed unattainable or refused by the patient, an alternative prosthesis must be designed, and the process repeated, until an acceptable treatment plan is agreed upon.
Close coordination between the surgeon, prosthodontist/restorative dentist, and laboratory technician, through each stage of pretreatment planning (examination, mounted study casts, 2-dimensional and 3-dimensional radiography, diagnostic wax ups and ideal provisional restorations) is essential. The information gained through these efforts can then be transferred to the surgical phase through the use of surgical guides or guided surgery to create the best opportunity to achieve an optimal final result.
Without this thorough and implant-specific approach the final result of the surgical or prosthetic treatment might be compromised resulting in an implant complication. The majority of prosthetic implant complications discussed in this article fall into three main categories:
1. Misalignment of implants
2. Fixed/removable prosthesis-related complications
3. Screw-joint complications
Misalignment of Implants as a Prosthodontic Complication
Improper implant placement is among the biggest problems encountered by clinicians. Prosthodontic complications arising from improper implant alignment commonly require treatment by a highly trained prosthodontist or restorative dentist. Some of these patient cases can be saved, while, unfortunately, others cannot.
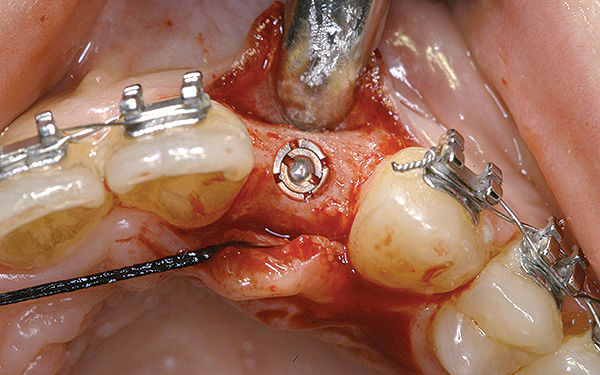
Although prosthodontists are capable of saving many complicated implant cases, the clinical results may still remain esthetically compromised. As opposed to heroic attempts to restore a misaligned implant, there are times when implant removal is a better solution. In the challenging case depicted in Figure 1 through Figure 4, it was determined that the implant, as positioned, could not be adequately restored. Two options were considered: implant removal and replacement with a properly positioned implant and implant replacement or submergence followed by the fabrication of a 3-unit fixed partial denture. The fixed partial denture would take advantage of utilizing tooth No. 8 as an abutment after removing the existing crown but would necessitate involving the virgin tooth No. 10. The surgical/prosthetic team in consultation with the patient elected to remove the implant and place a second implant. The implant was removed and a new implant was placed in the correct vertical and horizontal position using CT-guided surgery.
Similar complications can be seen in the case shown in Figure 5 and Figure 6, in which implants were placed too close together. Presurgical planning with the complete team might have considered the alternative of a cantilever prosthesis with one implant in either the central or lateral incisor position. In such situations an implant in the lateral position, if bone volume is available, is often the better alternative. With proper manipulation of the tissue in the ovate pontic central incisor, site development of papilla between the pontic No. 9, tooth No. 8 and implant No. 10 could be achieved with a high degree of success. It would also provide an excellent possibility to maintain proper papilla height between the implant and tooth No. 11, if the osseous crest was not compromised. By placing the implant in the lateral incisor position rather than in the central incisor position, if compromised interproximal bone height is present, an insufficient papilla height between the implant and adjacent tooth is relegated to the distal of the lateral incisor, a better esthetic alternative than between the central incisors.
Designing and creating a provisional restoration prior to implant placement can help assure excellent soft-tissue contour. A crucial element in the presurgical fabrication of a provisional restoration is finalizing the ideal position of the implant platform. This highlights the importance of collaboration between the prosthodontist and surgeon. Guided surgery can help the clinician transfer the planning to the patient. A well-planned case will result in the fabrication of an esthetic provisional restoration (Figure 7 through Figure 9). Based on the treatment planning information, the prosthodontist can have a prefabricated provisional restoration ready prior to implant placement. Small relining of the provisional restorations chairside and careful contouring of the soft tissue, using the provisional restoration, can result in an excellent emergence profile, resulting in an outstanding functional and esthetic outcome.
An example of complications arising in an otherwise functional implant is when the implant is incorrectly placed from a buccal-palatal aspect. As can be seen in Figure 10 and Figure 11, the prosthodontist was left with the challenge of developing a way to cover the implant that would be acceptable to the patient. The incorrect horizontal implant position left few options for improvement.
Fixed/Removable Prosthesis-Related Complications
UCLA abutments have given clinicians a better “exit strategy” when complications arise. The advantage of this type of abutment is its flexibility, which enables it to be customized. Today, fully customized abutments and milled computer-aided design/computer-aided manufacturing (CAD/CAM) abutments help clinicians save cases in more sophisticated ways.
The emergence profile of a single-tooth implant abutment has a significant effect on the esthetics of the final restoration. Digital technology offers the prosthodontist a variety of options, including having the ability to customize the abutment in order to fully match the natural emergence profile.
A 2010 article from the Journal of Dental Biomechanics compared a customized CAD/CAM abutment to standard abutments. The article pointed out that custom abutments have a stress value that is about 30% lower than standard abutments.1 This is clearly an advantage because the custom abutment causes less stress on the implant–abutment connection, placing less stress on the peri-implant bone.
In a case involving a 22-year-old woman with congenitally missing lateral incisors (Figure 12 through Figure 14), neither soft-tissue augmentation nor bone augmentation had been performed, resulting in a restorative challenge. However, a customized zirconia abutment helped create a natural emergence profile, which is still functioning well more than 10 years later. This case supports the authors’ opinion that zirconia abutments and restorations are preferable in esthetically challenging cases. Titanium abutments can be hidden without esthetic compromise if the patient has considerable soft-tissue thickness.2 However, digital technology has limitations in creating abutments of widely varying angulations.
Clinicians should adhere to recommended ratios of implant abutments and crowns to avoid long-term biomechanical problems. A progressive overload over time can cause an implant, abutment, or fixation screw to fracture. This often results in a screw coming loose, one of the most common prosthetic complications. Implant screw breakage is not quickly or easily managed. At times it may take hours for a clinician to remove a fractured screw. If an implant is damaged in the process, it may require removal.
There are many theories regarding the management of forces on implants. Excessive force is considered one factor contributing to peri-implant bone loss. A 2005 editorial reported a causal relationship “between the incidence of marginal bone loss next to an implant and occlusal overload.”3 It stated that a force-management approach is necessary. A 2013 Clinical Oral Implants Research article described a composite resin onlay bonded to a zirconia implant abutment, which presented “similar dynamic response to load when compared to teeth with simulated periodontal ligament.”4
A major topic of discussion in prosthodontics concerns restorative methods absorbing forces on implants. It is thought that this might contribute to the long-term success of the implant restoration. One possible option is a restoration made of a zirconia framework, with prefabricated composite veneers manufactured in a specific way, resulting in an extremely smooth surface to which plaque can only adhere to minimally. After the setup is finished, it is scanned, and the framework is designed on a computer. It is then milled, the veneers are bonded to the framework, and additional composite is added to individualize the final restoration. This is a very cost-efficient process, which is beneficial in satisfying the economic needs of many patients today.
Screw-Joint Complications
Beyond the difficulty in retrieving broken screws, there may be screw-joint complications exacerbated by full-zirconia abutments or titanium implants. A study from Sailer et al that compared four different groups of abutments, however, showed that the type of connection significantly influenced the abutment strength. Superior strength was achieved by means of an internal connection with a secondary metallic component.5 Due to the uncertainty of an adhesive’s longevity, the abutments could encounter long-term problems.
Concerning the implant–abutment interface, a biomechanics study by Hermann et al reported on the advantages of abutments that had been laser-connected to an implant as opposed to those that had been screwed to an implant. The investigators found that the “screwed” group lost significantly more bone than the “laser-connected” group, suggesting that implant–abutment stability is highly important in avoiding complications.6
Implants with a platform-switch design have both advantages and disadvantages related to stress. The design, which transfers stress from the implant–bone interface to the interior of the implant, relieves cortical bone strain but increases the strain and stress within the abutment, possibly leading to screw loosening or breaking. Therefore, if a platform-switch implant is used, a biomechanical, extremely stable implant–abutment connection is clearly favorable. The platform switch also provides clinicians with additional soft-tissue thickness to maximize esthetic results.
The esthetic advantage of a platform-switched implant with a customized zirconia abutment is demonstrated in the clinical case of a 24-year-old woman who received a provisional restoration after implant surgery (Figure 15 through Figure 19). The provisional was over-contoured, putting too much pressure on the peri-implant soft tissue. A soft-tissue necrosis developed due to inadequate blood supply to the affected area. The prosthodontist was able to save the case by using a customized zirconia abutment and a zirconia crown.
A report in the literature correlated problems with the depth of an implant margin with cement, noting that x-rays are not always a reliable method for cement evaluation.7 Our experience has shown cement-related implant problems as well. In an immediate-load study, the patient group with cemented provisional crowns demonstrated cement-related issues, while patients whose provisional restorations were screw-retained had no problems.8
While breakage associated with some materials is a prosthodontic problem, there are minimal failures or complications associated with materials produced via CAD/CAM. It is estimated that by 2017 US dentists will have placed more than 25 million CAD/CAM-manufactured crowns/bridges. Adoption of digital impression-taking systems and rapid prototyping/3-dimensional (3-D) printing will further fuel the dental prosthetics market to reach a value of more than $16.3 billion by 2017.9
Conclusions
Successful esthetic and functional restorations can, at times, be a challenge for prosthodontists when restoring dental implants. Patient expectations can be very high, putting demands on the surgical and restorative team. Implant positioning problems, fixed and removable prosthodontic problems, and material and mechanical considerations can make an ideal outcome more difficult to attain. Clearly, a multidisciplinary team approach optimizes implant treatment planning. The use of technology is essential in ensuring the accurate placement of components while minimizing complications. It also improves time management. Utilizing modern laboratory technology to create CAD/CAM restorations and employing such clinical technology as cone beam computed tomography (CBCT)-based virtual implant planning, stereolithographic-produced or milled surgical guides, and prefabricated provisional restorations can significantly reduce chair time and result in more cost-effective treatment with improved outcomes.
Prosthodontists not familiar with these technologies should take steps to evaluate, learn, and possibly integrate them into clinical practice.
About the Authors
Marcus Abboud, DMD, PhD
Associate Professor, Founding Chair, Department of Prosthodontics and Digital Technology, Stony Brook University, Stony Brook, New York
Leonard B. Kobren, DDS
Private Practice specializing in prosthodontics, White Plains, New York
Gary Orentlicher, DMD
Private Practice specializing in oral, maxillofacial, and implant surgery, Scarsdale, New York
References
1. Wu T, Liao W, Dai N, Tang C. Design of a custom angled abutment for dental implants using computer-aided design and nonlinear finite element analysis. J Biomech. 2010;43(10):1941-1946.
2. Jung RE, Sailer I, Hämmerle CH, et al. In vitro color changes of soft tissues caused by restorative materials. Int J Periodontics Restorative Dent. 2007;27(3):251-257.
3. Misch CE, Suzuki JB, Misch-Dietsh FM, Bidez MW. A positive correlation between occlusal trauma and peri-implant bone loss: literature support. Implant Dent. 2005;14(2):108-116.
4. Magne P, Silva M, Oderich E, et al. Damping behavior of implant-supported restorations. Clin Oral Implants Res. 2013;24(2):143-148.
5. Sailer I, Sailer T, Stawarczyk B, et al. In vitro study of the influence of the type of connection on the fracture load of zirconia abutments with internal and external implant-abutment connections. Int J Oral Maxillofac Implants. 2009;24(5):850-858.
6. Hermann JS, Schoolfield JD, Schenk RK, et al. Influence of the size of the microgap on crestal bone changes around titanium implants. A histometric evaluation of unloaded non-submerged implants in the canine mandible. J Periodontol. 2001;72(10):1372-1383.
7. Wadhwani C, Rapoport D, La Rosa S, et al. Radiographic detection and characteristic patterns of residual excess cement associated with cement-retained implant restorations: a clinical report. J Prosthet Dent. 2012;107(3):151-157.
8. Abboud M, Koeck B, Stark H, et al. Immediate loading of single-tooth implants in the posterior region. Int J Oral Maxillofac Implants. 2005;20(1):61-68.
9. Dental prosthetics and CAD/CAM market reaches upwards of $11 billion. Digital Manufacturing Report website. July 19, 2011. https://www.digitalmanufacturingreport.com/dmr/2011-07-19/dental_prosthetics_and_cad_cam_market_reaches_upwards_of_$11_billion.html. Accessed August 22, 2013.