Oral Diagnosis in the General Practice
Abstract
As dentistry moves into the medical and wellness model, the incorporation and proper utilization of appropriate advanced diagnostic technologies is essential. Today’s enhanced screening technologies range from computerized databases, to multi-spectrum visualization tools, to cell and tissue collection techniques. Properly communicating the benefits of the enhanced oral examination and other diagnostic procedures to patients and third-party payers may aid in the adoption and acceptance of these oral healthcare resources.
One of the primary goals for healthcare providers is to prevent disease and to arrest and even reverse the progression of any condition that is already present. A dental clinician’s most important function is the thorough assessment and evaluation of the patient’s oral and associated systemic health. An examination should not focus just on the dentition and the immediately surrounding periodontal tissue—the other structures and conditions of the oral cavity, head and neck, and systemic health are also vitally important. When examining the oral cavity, practitioners may overemphasize a single disease process, such as oral cancer, as the reason for the examination, rather than to ensure that all of the structures are healthy and within normal limits, and that any abnormality—whatever it may be—be discovered as early as possible. By effectively communicating examination and screening procedures, clinicians can greatly improve the perception of the importance of frequent and routine dental care.
The “loss leader” dental office promotions—free exams, free consultations—are often used to entice patients into a practice so more financially profitable procedures can be performed. These promotions have contributed to devaluating the perceived importance, benefit, and reimbursement of a complete and thorough examination for the patients, clinicians, and third-party payers such as insurance providers alike. This downplaying of the significance of a comprehensive and enhanced examination misrepresents the substantial amount of knowledge, technology, and expertise required to perform these valuable procedures properly.
Patients who believe that the primary importance of a preventive dental/hygiene appointment is to prevent decay and maintain a beautiful smile have missed the real value of a thorough oral examination. Unfortunately, the patient’s perception often is that the primary goal of a check-up is to find a problem which will cost money to fix. However, clinicians who are routinely performing an enhanced head and neck examination, including a tactile exam and an enhanced visual inspection of the oral mucosal tissue using today’s advanced technologies, have the opportunity to change patients’ perceptions.
The Enhanced Examination
The enhanced comprehensive head and neck examination is a multifaceted procedure with many steps (Table 1). It requires general practitioners to have the knowledge, communication skills, and technical expertise to properly assess every patient in their care. Today’s enhanced screening technologies range from computerized databases, to multi-spectrum visualization tools that allow practitioners to see deeper into soft tissue, to simplified cell and tissue collection techniques. No single modality can deliver 100% accuracy or effectiveness in detecting conditions. Screening and diagnosis is accomplished with the accumulation of data from multiple procedures and sources. Today’s screening and diagnostic aids can have a significant impact on the assessment of a patient’s health and well being.
A patient’s health, pharmacological history, and current status are the foundation of the examination process. Because patients’ systemic and dental health situations are becoming increasingly more complex—with an expanding number of medications—the need for computerized pharmacology and medical condition databases to assist in the patient assessment process is greater than ever. With more than 800 medications that have a xerostomic effect and more than 400 drug formularies changing weekly, clinicians require computerized assistance to stay current. Internet-based systems such as the Lexi-Comp Dental Reference Library™ (Lexi-Comp, Inc., www.lexi.com) provide a collection of interactive databases and reference manuals continually updated as the FDA and drug manufacturers announce changes to their drug information and systemic conditions, with a specialized focus on their relationship to dentistry. This database is designed to allow dental professionals quick and easy access to critical information on drug interactions that influence oral conditions. Its orientation to dental-specific applications helps ensure the correct diagnosis and appropriate care are rendered for each patient’s situation. The complete library also includes a reference manual for the diagnosis and management of oral soft-tissue diseases, providing information on the most common oral conditions divided into sections based on visual appearance (with images of the abnormalities), which assists clinicians in establishing the differential diagnosis. Once a clinical working diagnosis has been attained, suggestions are presented for possible treatment and management.
The demographics, risks, and etiological factors that relate to head and neck cancer and other mucosal abnormalities have changed in recent years. These changes call for enhanced head and neck and oral examinations on all adult patients and others with special considerations (Table 2). The frequency of human papillomavirus (HPV)-positive oropharyngeal squamous cell carcinoma (OPSCC) is consistently unassociated with dysplasias of the surface epithelium; cervical lymphadenopathy is often the first clinically detectable sign. Thus, it is extremely important that oral healthcare providers carefully perform an extensive extraoral head and neck examination, especially of all cervical lymph nodes.1
Visual Enhancements for Soft Tissue Evaluation
Visual examination with a standard white light has been the cornerstone of a comprehensive examination. Any noninvasive device that improves the clinician’s visualization and ability to achieve early detection of soft-tissue abnormalities, especially those that are neoplastic in nature, is an invaluable asset to the diagnostic armamentarium. Any visual enhancement device should be used in combination with a conventional visual oral mucosal examination to improve the evaluation, identification, and monitoring of oral mucosa and abnormalities. Available imaging modalities include the use of reflectance and fluorescence technology to evaluate tissue under various illumination conditions.
Fluorescence technology, in particular, is a noninvasive approach for assessing and aiding in the visualization of chemical and morphological patterns of the various tissues and substances within the oral cavity.2 Fluorescence visualization enhances the clinician’s ability to observe changes in these patterns and can aid in evaluating both the hard- and soft-tissue structures, as well as the biological activity of the flora and other microbial activity. These technologies do not require the use of any mouth rinses or stains; the process simply repeats the visual exam with the aid of the device(s).
Products such as the VELscope Vx™ (LED Dental Inc., www.velscope.com) and the DentLight Oral Exam Light Kit (DentLight Inc., www.dentlight.com) enable clinicians to visually scan the entire oral cavity for changes in the fluorescence pattern of tissue, which may indicate an area of concern.
The Identafi® (DentalEZ Group, www.dentalez.com) oral cancer screening device uses a multispectral fluorescence and reflectance technology to enhance visualization of mucosal abnormalities. The small, cordless handheld device uses a three-wavelength optical illumination and visualization system that allows dental professionals to identify oral mucosal abnormalities. Identafi’s three separate wavelengths of light—white, violet, and green-amber—excite oral tissue, providing the clinician three different illumination perspectives to visualize the area being examined. A disposable mirror attachment assists in visualizing the area in an indirect manner.
When an area of concern is discovered through this examination, the clinician needs to ask the appropriate questions to help ascertain the potential cause and the proper course of action. Having a comprehensive understanding of how the technology responds to various conditions, as well as knowledge of the disease processes, will help guide the practitioner to successful outcomes. The clinician must develop a systematic and science-based methodology for handling all of the findings. This underscores the need for thorough education on all the technologies that are being incorporated.
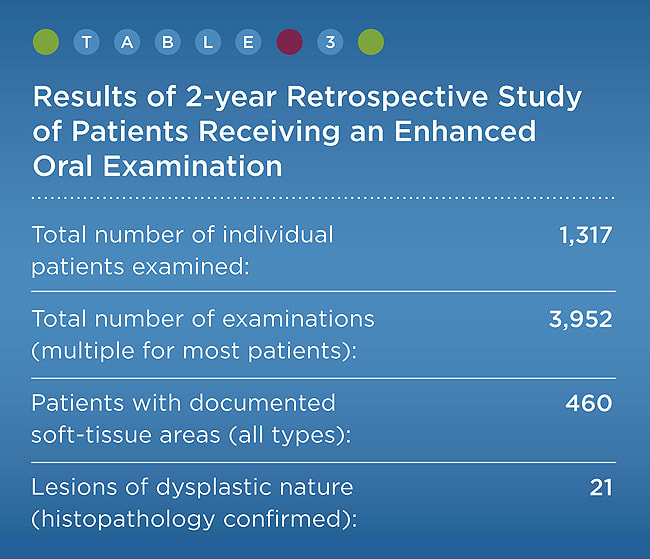
In a retrospective study with 1,317 patients receiving enhanced oral mucosal examination with the use of fluorescence visualization in a private general dental practice over a 2-year period, 460 of the patients (approximately 35%) had a soft-tissue abnormality that was noted in the clinical record. Although none of these patients were diagnosed with oral cancer, 21 of the patients had lesions that were confirmed by a full-thickness biopsy to be dysplastic in nature3 (Table 3). The patients with dysplasia were educated on the potential risks of transformation into oral squamous cell carcinoma (OSCC) and advised to eliminate risk factors where possible. These patients were also educated on the need for ongoing surveillance of their condition and scheduled for the enhanced mucosal examination with fluorescence visualization to monitor the condition’s progression or regression on a 3-month recall basis. The remaining patients with soft-tissue abnormalities were counseled and, when appropriate, minor corrective actions were taken and treatment was provided to manage the area of concern. As part of the discussion about proper case management, the need for regular ongoing preventive dental care and surveillance was reinforced.
Unfortunately, research has not yet been able to determine which lesions of dysplastic nature will progress into OSCC, and which ones will remain in a dysplastic state or regress back to a normal state. As previously stated, the goal of hygienists and general practitioners is to discover any abnormalities as early in the disease process as possible: This facilitates early intervention when appropriate in an attempt to limit the progression and enable regression.
Microscopic Evaluation and Cytology
Full-thickness surgical biopsy with a microscopic examination is the accepted method of diagnosing cancer and many other mucosal conditions. The role of a biopsy is to rule out a malignancy and to establish the appropriate diagnosis for the patient’s condition. All other modalities, including toluidine blue staining and cytology, are adjunctive procedures to aid in determining if and where a surgical biopsy would be appropriate and most beneficial. Staining and cytology are not substitutes for the traditional “gold standard” surgical biopsy technique of removing architecturally intact tissue. In the majority of cases, a lesion that is worthy of a staining or cytology procedure may be better served by a surgical biopsy that will render a diagnosis.
Another adjunctive screening procedure, brush cytology, involves the collection of transepithelial mucosa cells by means of a minimally invasive sterile, plastic-handled nylon bristle brush—with little or no discomfort to the patient. Disaggregated epithelial cells are acquired by vigorous brushing of the oral lesion with a sterile nylon bristle brush. This technique is used primarily to screen a suspicious leukoplakia or erythroplakia of the mouth in order to aid in determining the presence or lack of premalignant dysplastic change. Brush cytology is an effective system for ruling out the presence of abnormal, atypical, and dysplastic cells in areas that have been properly brushed. The cells are transferred to and fixed on a glass slide or placed in a special liquid preservative/fixative in a bottle; the collected sample is then sent to the laboratory for processing and histological evaluation.
The use of liquid-based cytology in the oral cavity is a relatively new screening technique that has also been proven effective when an area of abnormality has been discovered. Not only can it be used for the detection of dysplastic cells, but it also can be used to detect other oral conditions such as herpes simplex infection and candidiasis. Brush cytology may also aid the clinician in determining if the lesion detected should be observed or treated, or if an immediate invasive full-thickness biopsy procedure with intact architecture should be performed.
Salivary diagnostics has become a reality: patients rinse with specialized solutions and expectorate into a funneled collection tube that is processed and analyzed at the laboratory. Due to the simplicity and noninvasive nature of salivary collection and testing, these screening modalities strongly appeal to clinicians. The saliva that is collected can be evaluated at the laboratory for the status and susceptibility to both oral and systemic conditions. OralDNA® Labs (www.oraldna.com) has developed salivary tests to determine the patient’s genetic susceptibility to and inherent risk of periodontal disease, as well as a test to identify the type and concentration of 13 pathogenic bacteria that are known to cause periodontal disease. The company’s OraRisk® HPV test is another noninvasive salivary screening tool to help identify patients who might be at an increased risk for oropharyngeal cancer and to assist in developing the appropriate referral and surveillance recommendations.
Communicating Value
The entire dental team plays a strategic role in the data collection, discovery, diagnostic process, and management (Figure 1). From the patient’s very first contact with the dental office, whether it is on the phone, over the practice’s internet portals, or in person, the importance of a consistent message on the value and necessity of an enhanced oral examination cannot be overstated. Properly communicating the real purpose of these procedures is extremely important in changing patients’ perceptions of the enhanced examination techniques and helping them realize the significant benefits involved.
Effective communication is a critical component of the examination process. When clinicians inaccurately state that they are going to do an “oral cancer exam,” it implies that cancer is the only thing they are looking for. After they have explained it in this manner, no matter how clinicians present their findings, it can cause the patient undue anxiety. If any abnormality is found the patient often perceives it as possibly cancer, especially if the area of concern requires follow-up attention or treatment.
The goal of an enhanced examination and screening is to discover any abnormality, no matter what it may be. A more appropriate way to present and discuss the exam with patients is to tell them that an enhanced oral evaluation is going to be done, in which all of their teeth and surrounding structures will be examined, and everything will be checked, from cavities, to cheek bites, to cancer.
When incorporating any new technology into a dental practice, education and training that encompasses the entire dental team is crucial to understanding specific technologies, their true role and value, and, even more importantly, their limitations. Because most patients first turn to the office’s staff for advice and comforting regarding a procedure, the value of education for the entire team cannot be overstated.
Conclusion
The significance of the diagnostic process continues to be undervalued by patients and clinicians alike. Despite the fact that there is an ADA code on dental procedures and nomenclature (CDT) for an “adjunctive pre-diagnostic test,” the lack of insurance coverage impedes the adoption and acceptance of these advanced diagnostic technologies and procedures. However, it is the practitioner’s responsibility to use all modalities that are reasonably available to accomplish the best outcomes for the patients.
The incorporation and proper utilization of appropriate advanced diagnostic technologies is essential as dentistry moves forward into the medical and wellness model. Understanding and properly communicating the full benefit that the enhanced examination and other diagnostic procedures will provide for the patient is imperative. After all, the goal of all healthcare professionals is to facilitate better patient outcomes and to enhance and improve the patient’s quality of life.
Disclosure
The author is a shareholder in LED Medical Diagnostics, Inc.
References
1. Kahn M. The emerging role of human papillomavirus in oropharyngeal squamous cell carcinoma. Compend Contin Educ Dent. 2011:32(Spec Iss 2):1-7.
2. Gillenwater A, Jacob R, Ganeshappa R, et al. Noninvasive diagnosis of oral neoplasia based on fluorescence spectroscopy and native tissue autofluorescence. Arch Otolaryngol Head Neck Surg. 1998;124(11):1251-1258.
3. Benjamin SD. The role and responsibilities of the general dental practice. The inside summit on oral cancer discovery and management. The technologies and the role of dental clinicians. Inside Dentistry. 2007;3(S2):23-25.
About the Author
Scott D. Benjamin, DDS
Private Practice
Sidney, New York