John M. Powers, PhD; and John W. Farah, DDS, PhD
Amilling center is often the link between the dentist and dental laboratory when the dentist prescribes a zirconia-based ceramic restoration for a patient. The milling center is a central resource consisting of skilled technicians, scanners, margin marking and coping design software, milling equipment, and sintering furnaces.1 Various materials, including silica-based ceramics, zirconia-based ceramics, metal alloys, polymers, and wax, can be milled to form copings, frameworks, or patterns for final restorations.2
The milling center can accept traditional elastomeric impressions and gypsum dies or digital data from various chairside and laboratory scanners. With traditional gypsum dies, digital information is obtained by laboratory scanners. Chairside oral scanners provide digital data that can be used by the milling center for design and milling and by a stereolithography (SLA) center to produce an SLA die.3 If desired, the SLA die can be used by the dental laboratory to produce traditional alloy castings or pressed ceramic restorations.
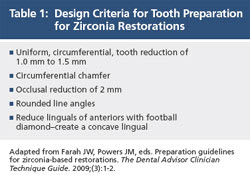
Tooth preparation is critical for a successful zirconia restoration: guidelines for tooth preparation are listed in Table 1.4 Tooth reduction for zirconia crowns is less than that required for ceramic–metal or all-ceramic restorations because zirconia has high strength and does not require an opaquing layer. If a digital impression is made, the margins must be completely revealed.
The production of a ceramic veneer for a zirconia restoration by the dental laboratory requires techniques that differ from those associated with ceramic–metal restorations. Table 2 lists tips for the dental laboratory producing zirconia restorations.5 The goal is to minimize chipping and fractures of the veneering ceramic caused by improper design and processing. An important design factor is to maintain 1.5 mm or less thickness of veneering ceramic by designing an anatomic zirconia coping. A second factor is to select a veneering ceramic with a coefficient of thermal expansion (about 9.1 to 10.2 x 10-6/K) that is compatible with the zirconia being used. A third factor is to employ slow heating and cooling rates (about half those used with porcelain-fused-to-metal [PFM]) during the veneering process because zirconia is a poor thermal conductor compared to metal alloys.
The milling center has a number of challenges related to the production of zirconia copings and frameworks as described in Table 3. The most notable issue is difficulty in margin marking resulting from less-than-ideal or unclear margins or die trimming that leaves margins that are ambiguous or too sharp. Another challenge is chipping during milling of the zirconia, caused by design, burs, margin reinforcement, or billet material.
Clinical Research
Results of a clinical study published in The Dental Advisor Research Report comparing the fit of zirconia restorations made by digital impressions vs traditional addition silicone impressions are listed in Table 4.6 Researchers enrolled 61 patients who needed full-coverage restorations. A total of 63 teeth were prepared. Digital scans (Lava™ Chairside Oral Scanner C.O.S., 3M™ ESPE™, https://www.3mespe.com) were obtained to design the crown and to produce an SLA model for use by the dental laboratory. In addition to the digital scan, upper and lower impressions (Aquasil Ultra, DENTSPLY Caulk, https://www.caulk.com) (putty or heavy body with light body) with a bite registration were performed for each patient. The elastomeric impressions were handled traditionally for the production of stone models and dies. Two zirconia copings (Lava Crowns and Bridges, 3M ESPE) were fabricated for each prepared tooth for a total of 126 restorations. After comparing the fit of each crown intraorally, 71% of the Lava C.O.S. crowns and 29% of the impression crowns were cemented.
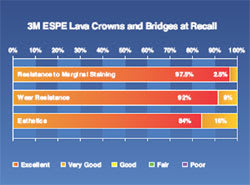
Results of a 6-year clinical study of zirconia restorations (Lava Crowns and Bridges) have been reported in The Dental Advisor (Figure 1).7 At 6 years, 640 restorations were evaluated. Fractures of the ceramic veneer that required replacement were 3.8% (Figure 2). Chipping that necessitated smoothing and polishing were 6.1%. A total of 84% of the restorations had excellent shade match with the remainder rated “very good.” Only 2.5% of the restorations exhibited slight graying at the margins. Ninety-two percent of the restorations exhibited no wear while 8% exhibited slight wear of the ceramic veneer. Minimal wear was noted in 17% of the opposing teeth.
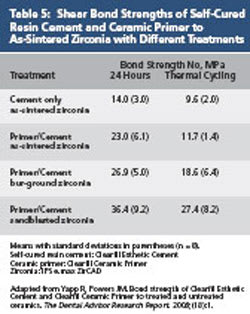
Cementation of zirconia restorations with good retention can be accomplished with self-adhesive resin cements.8 Zirconia restorations with poor retention should be bonded using a bonding agent, resin cement, and ceramic primer formulated for zirconia.9 Shear bond strengths of self-cured resin cement (Clearfil Esthetic Cement, Kuraray America, https://www.kuraraydental.com) and ceramic primer (Clearfil Ceramic Primer, Kuraray America) to as-sintered zirconia (IPS e.max® ZirCAD, Ivoclar Vivadent, https://www.ivoclarvivadent.us) with different treatments are listed in Table 5.10
Results of a 6-year clinical study of self-adhesive resin cement (RelyX™ Unicem Self-Adhesive Universal Resin Cement, 3M ESPE) have been reported in The Dental Advisor (Figure 3).11 More than 5600 restorations were cemented during a 6.5-year period, and 1739 restorations were available for evaluation. These included all-ceramic inlays, onlays, crowns, bridges, PFM crowns and bridges, posts, and computer-aided design and computer-aided manufacturing (CAD/CAM) restorations. Postoperative sensitivity was less than 1.2% of the seated restorations and usually occurred in the first year after cementation. Graying at the margins was noted in 5.3% of the restorations and was time related. Some of the restorations (1.3%) needed to be replaced as a result of the graying. A low debonding rate of 2.6% was documented during the 6-year evaluation period. Among the evaluated restorations, 46 required re-cementation, including 24 ceramic onlays, 10 ceramic crowns, and 12 PFM crowns. Of the 24 ceramic on-lays that debonded, 12 had little direct retention. In five of these debonding cases, a portion of the tooth fractured.
Conclusion
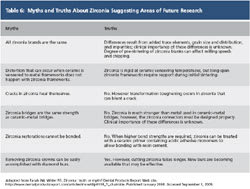
Successful zirconia restorations require attention to proper techniques for tooth preparation, impressioning, design, milling, ceramic veneering, and cementation. There is still much to learn about zirconia and the production of zirconia copings and frameworks. Some truths and myths are described in Table 6.12
Disclosures
The authors have a financial interest in Dental Consultants, Inc (publisher of The Dental Advisor) and Apex Dental Milling (Authorized Lava Milling Center and Dental Mill-Crystal). Research funding was supported in part by 3M ESPE, Kuraray America, and Ivoclar Vivadent.
Acknowledgments
The authors would like to acknowledge Ron Yapp, MS; Chris Brown, BSEE; and Robert S. Wisler, CDT for their suggestions and collaboration.
References
1. Farah JW, Powers JM, eds. CAD/CAM dentistry. The Dental Advisor. 2008;25(9):1-7.
2. Farah JW, Powers JM, eds. Zirconia-based ceramics. The Dental Advisor. 2007;24(10):1-6.
3. Farah JW, Reed C, Wojtowicz D. 3M ESPE Lava Chairside Oral Scanner C.O.S. The Dental Advisor Clinical Case Report. 2009;(10):1-3.
4. Farah JW, Powers JM, eds. Preparation guidelines for zirconia-based restorations. The Dental Advisor Clinician Technique Guide. 2009;(3):1-2.
5. Zirconia-supported ceramic restorations: uncovering the mysteries. Espertise Scientific Facts. St. Paul, MN: 3M ESPE; 2009.
6. Farah JW, Brown L. Comparison of the fit of crowns based on digital impressions with 3M ESPE Lava Chairside Oral Scanner C.O.S. vs. traditional impressions. The Dental Advisor Research Report. 2009;(22):1-3.
7. Farah JW, Powers JM, eds. Update on CAD/CAM dentistry. The Dental Advisor. 2009;26(7):14-15.
8. Powers JM, O’Keefe KL. Guide to Zirconia Bonding Essentials. New York, NY: Kuraray America, Inc; 2009:1-13.
9. Yapp R, Powers JM. Bond strength of resin cement to treated zirconia. The Dental Advisor Research Report. 2008;(19):1.
10. Yapp R, Powers JM. Bond strength of Clearfil Esthetic Cement and Clearfil Ceramic Primer to treated and untreated ceramics. The Dental Advisor Research Report. 2008;(18): 1.
11. Farah JW, Powers JM, eds. Esthetic fiber posts. The Dental Advisor. 2009;26(5):6-7.
12. Farah JW, Wisler RS. Zirconia: truth or myth? Dental Products Report Web site. https://www.dentalproductsreport.com/articles/show/dlp0108_ft_chairside. Published January 2008. Accessed September 1, 2009.
Figure 1 | Figure 1 Results of a 6-year clinical study of zirconia restorations (Lava Crowns and Bridges). Farah JW, Powers JM, eds. Update on CAD/CAM dentistry. The Dental Advisor. 2009; 26(7):14-15. Reprinted by permission of Dental Consultants, Inc. | ||||||
Figure 2 Fracture and chipping of veneering ceramic in 6-year clinical study of zirconia restorations (Lava Crowns and Bridges). Farah JW, Powers JM, eds. Update on CAD/CAM dentistry. The Dental Advisor. 2009;26(7):14-15. Reprinted by permission of Dental Consultants, Inc. | Figure 3 Results of a 6-year clinical study of a self-adhesive resin cement (RelyX Unicem Self-Adhesive Universal Resin Cement). Farah JW, Powers JM, eds. Esthetic fiber posts. The Dental Advisor. 2009;26(5):6-7. Reprinted by permission of Dental Consultants, Inc. | ||||||
Table 1 | Table 6 | ||||||
Table 2 | Table 3 | ||||||
Table 4 | Table 5 | ||||||
| |||||||