Jin-Ho Phark, DDS; Sillas Duarte Jr, DDS, MS, PhD; Hendrik Meyer-Lueckel, DDS, PhD, MPH; Sebastian
Abstract: Noninvasive (preventive) measures involving fluoridation, dietary control, and oral hygiene instruction, as well as invasive restorative methods, are the standard treatment options for interproximal caries. Intermediate treatment options, similar to pit-and-fissure sealing on occlusal surfaces that has been shown to be effective in preventing and inhibiting caries, have not yet been established on interproximal surfaces. Recently, the application of resins on interproximal caries lesions has been studied and improved, leading to the development of new materials, which infiltrate and seal the carious lesion, improving the inhibition of caries progression. Clinical data show this new technique complements existing treatment options for interproximal caries by delaying the time point for a restoration and consequently closing the gap between noninvasive and invasive treatment options.
Abstract: Noninvasive (preventive) measures involving fluoridation, dietary control, and oral hygiene instruction, as well as invasive restorative methods, are the standard treatment options for interproximal caries. Intermediate treatment options, similar to pit-and-fissure sealing on occlusal surfaces that has been shown to be effective in preventing and inhibiting caries, have not yet been established on interproximal surfaces. Recently, the application of resins on interproximal caries lesions has been studied and improved, leading to the development of new materials, which infiltrate and seal the carious lesion, improving the inhibition of caries progression. Clinical data show this new technique complements existing treatment options for interproximal caries by delaying the time point for a restoration and consequently closing the gap between noninvasive and invasive treatment options.
Treatment of interproximal caries usually is limited to two choices: noninvasive (preventive) or invasive (restorative). Noninvasive measures include application of fluorides in combination with improvement of a patient’s oral hygiene and dietary control to prevent lesion formation (primary prevention) or to enhance lesion remineralization and arrest lesion progression (secondary prevention) (Figure 1). However, this approach is dependent on good patient compliance. Moreover, for proximal surfaces with surface breakdowns, this method will probably fail because the patient can no longer clean the lesion surfaces sufficiently.1 Thus, a rather slow but continuous progression of these lesions has been reported even under controlled preventive conditions.2 When noninvasive measures are ineffective, invasive intervention is indicated. Unfortunately, for interproximal surfaces in particular, large areas of sound enamel have to be removed even with minimally invasive preparation techniques. In addition, different treatment philosophies lead to diverse recommendations for the timing of invasive treatment. Therefore, the decision between the two treatment methods is often difficult, especially for lesions radiographically extending just to the dentoenamel junction (Figure 1).3 Often, invasive treatment is performed too early, because intermediate treatment options, similar to pit-and-fissure sealing on occlusal surfaces, are not established yet for interproximal surfaces. Recently, a new technique for treating interproximal caries lesions has been described.4,5 In this microinvasive approach, called resin infiltration, noncavitated caries lesions are infiltrated with a low-viscosity resin. This technique might be a useful addition to the treatment options of interproximal caries, possibly delaying invasive treatment for several years.
Resin Sealing of Caries Lesions
Sealants have been used successfully to prevent caries on occlusal surfaces.6 They also have been employed therapeutically on noncavitated occlusal caries, where they are effective in reducing caries progression.7 Ultimately, arresting caries by sealants was applied to interproximal smooth surfaces. After temporary tooth separation and surface etching with phosphoric acid dental adhesives, sealants or resin patches were bonded to the lesions to act as diffusion barriers.8-10 For interproximal sealing with adhesives, clinical results showed a significant reduction of lesion progression.9
Resin Infiltration of Interproximal Caries Lesions
In enamel caries, the pores in the subsurface lesion body act as diffusion pathways for organic acids and minerals,11 leading to the dissolution of enamel at the advancing front of the lesion. Therefore, occlusion of these pores by penetration with low-viscosity light-curing resins might arrest lesion progression. In contrast to caries sealing where a superficial resin coat is created, the caries infiltration technique establishes a barrier within the caries lesions themselves that could strengthen the enamel structure, thus preventing cavitation or break-down of the enamel surface.
Various researchers have evaluated the penetration of artificial and natural lesions with commercially available adhesives or experimental resins in vitro.8,12-19 Some of these studies showed the penetration of adhesives into artificially demineralized enamel lesions inhibited the progression of the lesions even during repeated demineralization. In some studies8,12,13,16-19 that involved adhesives or fissure sealants in the form of a surface sealant, it was unclear whether the demineralization-inhibiting effect was caused by the penetration of the resin into the enamel pores or by simply covering the surface with resin. Recent in vitro studies, in which the excess resin material was removed from the lesion surface, clearly demonstrated the resin that infiltrated the enamel pores was able to inhibit caries progression.14,15 To achieve good adhesion and penetration of the resin into the more porous subsurface lesion body of the artificial lesions, the pseudo-intact surface layer was etched using phosphoric acid.16 This layer is formed by precipitation of minerals on the enamel surface and has a much lower pore volume compared to the lesion body, thus inhibiting the penetration of the resin. However, there are structural differences between artificial and natural enamel lesions. The surface layers of natural lesions are more inhomogeneous and may show greater thickness and mineral content compared to artificial lesions because of alternating demineralization and remineralization cycles in the oral cavity.20 Therefore, penetration of adhesives into natural lesions even after 2 min of etching with phosphoric acid was only superficial.4,13 For that reason, an alternative etching protocol using 15% hydrochloric acid for 2 min was developed.21 In addition, the rheologic properties of regular adhesives do not allow sufficient penetration into the porous lesion. Therefore, resins with low viscosity (infiltrants) with improved rheologic properties were developed.22-24 The combination of etching with hydrochloric acid and the application of low-viscosity infiltrants allowed a nearly complete penetration of natural enamel carious lesions (Figure 2).5,25 Hydrochloric acid has been used in dentistry for microabrasion in concentrations up to 18% combined with pumice or silica particles.26,27 Microabrasion eroded and abraded up to 360 ± 130 µm of enamel within 100 sec;28 it needed to be applied repeatedly up to total of 9 min.29 Etching for resin infiltration using a 15% hydrochloric acid gel for 2 min removed less than 30 µm of demineralized and sound enamel.21 Due to the caustic nature of hydro-chloric acid30 appropriate soft tissue isolation, eg, rubber dam or light curing barrier material, is required.
Clinical studies examining the application of infiltrating resin on interproximal surfaces of primary and permanent teeth, as well as on post-orthodontic white spots on facial surfaces, are ongoing. Initial results from three studies (unpublished data) evaluating the efficacy and safety of resin infiltration show a significantly reduced lesion progression for infiltrated lesions extending radiographically into inner enamel or outer third of dentin compared to untreated control lesions after 12 to 18 months.
Clinical Application
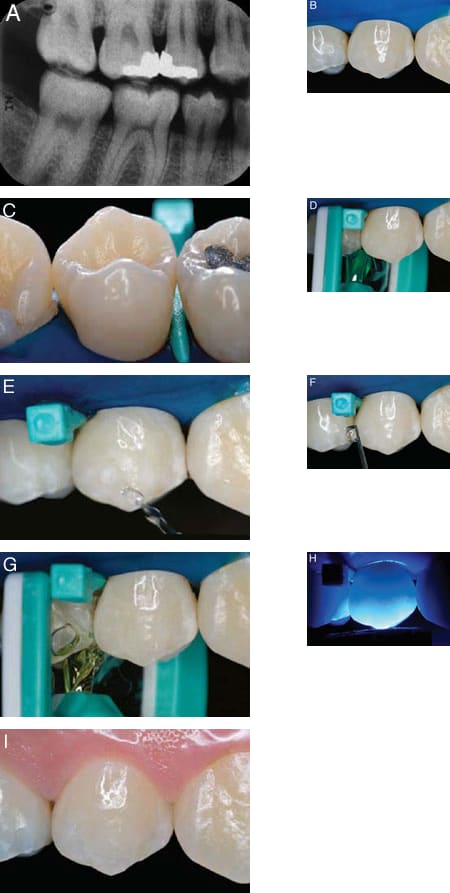
Accessibility is a key factor during clinical application of sealing or infiltration of interproximal caries lesions (Figure 3 and Figure 4). In studies focusing on sealing the interproximal lesions, orthodontic elastics, usually placed several days before the actual treatment visit, have been used to separate the teeth. After field isolation with cotton rolls or rubber dam, the adjacent tooth surface was protected with a matrix band or Teflon tape, followed by etching with phosphoric acid for 60 sec, water rinsing, and air drying. Then the adhesive, sealants, and resin patches were applied, light-cured, and polished with polishing strips.8-10
For resin infiltration, rubber dam is applied (Figure 5B). Then the teeth are separated for up to 40 µm with a flattened wedge. The design of the wedge allows access to the interproximal lesion for treatment without covering it (Figure 5C). Due to the minimal and thus atraumatic amount of necessary separation, the treatment can be applied in the same session. Between the separated teeth a special applicator (Figure 3) is inserted. The applicator consists of two parallel foils. One foil has microperforations, which face the lesion, and the other foil has no perforations, facing the adjacent proximal tooth surface. The applicator’s design helps deliver the materials needed for treatment through the perforations precisely to the lesion and helps protect the adjacent tooth surface on the non-perforated side from unintended contamination with the applied materials. The treatment starts with the application of hydrochloric acid etching gel for 2 min to erode the surface layer of the lesion (Figure 5D). Then, after water rinsing (Figure 5E), ethanol application (Figure 5F), and air drying, the infiltrant is applied (Figure 5G). After 3 min of application the infiltrant has penetrated into the lesion deep enough. Excess resin material is removed with a gentle air blow, thus leaving no overhang, which could cause plaque retention or secondary decay. Once the resin is light cured (Figure 5H) a second coat is applied for only 1 min in the same way. The infiltrated lesion 1 week after treatment is shown in Figure 5I. To date, the infiltrating resin does not contain any radiographic markers, therefore immediate posttreatment control of penetration depth is not available. Similar to occlusal sealing techniques, treatment success can be determined mainly by monitoring inhibition or decrease of caries progression during follow-up examinations.3
For treatment of postorthodontic white spots, the steps are identical to the interproximal application, except for the location of the lesions and the use of a different applicator (Figure 4). For soft-tissue isolation light curing barrier material can be used as an alternative to rubber dam. In addition to inhibiting caries progression, resin infiltration can esthetically improve postorthodontic white spots (Figure 6). This technique might be applicable during orthodontic treatment on white spots around fixed appliances, as well.
Conclusion
New treatment techniques for interproximal caries by sealing/infiltrating the lesion surface efficaciously inhibit caries progression. These techniques close the therapeutic gap between noninvasive (preventive) and invasive treatment options for inter-proximal caries. For caries lesions on interproximal and facial smooth surfaces, the application of infiltrating resins might significantly postpone the first invasive intervention.
Disclosure
Dr. Phark has received a research grant from DMG. Dr. Meyer-Lueckel and Dr. Paris have received a research grant and royalties from DMG, as well as a research grant from the Deutsche Forschungsgemeinschaft, DFG (PA1505/1-1).
About the Authors
Jin-Ho Phark, DDS
Assistant Professor, Department of Comprehensive Care, School of Dental Medicine, Case Western Reserve University, Cleveland, Ohio
Sillas Duarte Jr, DDS, MS, PhD
Associate Professor, Department of Comprehensive Care, School of Dental Medicine, Case Western Reserve University, Cleveland, Ohio
Hendrik Meyer-Lueckel, DDS, PhD, MPH
Associate Professor, Clinic for Conservative Dentistry and Periodontology, School of Dental Medicine, Christian-Albrechts-Universität zu Kiel, Germany
Sebastian Paris, DDS
Assistant Professor, Clinic for Conservative Dentistry and Periodontology, School of Dental Medicine, Christian-Albrechts-Universität zu Kiel, Germany
References
1. Ratledge DK, Kidd EA, Beighton D. A clinical and microbiological study of approximal carious lesions. Part 1: the relationship between cavitation, radiographic lesion depth, the site-specific gingival index and the level of infection of the dentine. Caries Res. 2001;35(1):3-7.
2. Mejàre I, Källestål C, Stenlund H, Johansson H. Caries development from 11 to 22 years of age: a prospective radiographic study. Prevalence and distribution. Caries Res. 1998;32(1):10-16.
3. Meyer-Lueckel H, Fejerskov O, Paris S. Novel treatment options for proximal caries [in German]. Schweiz Monatsschr Zahnmed. 2009;119:454-461.
4. Paris S, Meyer-Lueckel H, Kielbassa AM. Resin infiltration of natural caries lesions. J Dent Res. 2007;86(7):662-666.
5. Meyer-Lueckel H, Paris S. Improved resin infiltration of natural caries lesions. J Dent Res. 2008;87(12): 1112-1116.
6. Mejàre I, Lingström P, Petersson LG, et al. Caries-preventive effect of fissure sealants: a systematic review. Acta Odontol Scand. 2003;61(6): 321-330.
7. Griffin SO, Oong E, Kohn W, et al. The effectiveness of sealants in managing caries lesions. J Dent Res. 2008;87(2):169-174.
8. Schmidlin PR, Zehnder M, Pasqualetti T, et al. Penetration of a bonding agent into de- and remineralized enamel in vitro. J Adhes Dent. 2004;6(2):111-115.
9. Martignon S, Ekstrand KR, Ellwood R. Efficacy of sealing proximal early active lesions: an 18-month clinical study evaluated by conventional and subtraction radiography. Caries Res. 2006;40(5):382-388.
10. Gomez SS, Basili CP, Emilson CG. A 2-year clinical evaluation of sealed noncavitated approximal posterior carious lesions in adolescents. Clin Oral Investig. 2005;9(4):239-243.
11. ten Cate JM, Larsen MJ, Pearce EIF, et al. Chemical interactions between the tooth and oral fluids. In Fejerskov O, Kidd E, eds. Dental Caries: The Disease and its Clinical Management. Ames, IA: Blackwell Munksgaard; 2003:49-68.
12. Robinson C, Hallsworth AS, Weatherell JA, Künzel W. Arrest and control of carious lesions: a study based on preliminary experiments with resorcinol-formaldehyde resin. J Dent Res. 1976;55(5):812-818.
13. Davila JM, Buonocore MG, Greeley CB, Provenza DV. Adhesive penetration in human artificial and natural white spots. J Dent Res. 1975;54(5):999-1008.
14. Paris S, Meyer-Lueckel H, Mueller J, et al. Progression of sealed initial bovine enamel lesions under demineralizing conditions in vitro. Caries Res. 2006;40(2):124-129.
15. Meyer-Lueckel H, Paris S, Mueller J, et al. Influence of the application time on the penetration of different dental adhesives and a fissure sealant into artificial subsurface lesions in bovine enamel. Dent Mater. 2006;22(1):22-28.
16. Gray GB, Shellis P. Infiltration of resin into white spot caries-like lesions of enamel: an in vitro study. Eur J Prosthodont Restor Dent. 2002;10(1): 27-32.
17. Goepferd SJ, Olberding P. The effect of sealing white spot lesions on lesion progression in vitro. Pediatr Dent. 1989;11(1):14-16.
18. Garcia-Godoy F, Summitt JB, Donly KJ. Caries progression of white spot lesions sealed with an unfilled resin. J Clin Pediatr Dent. 1997;21(2):141-143.
19. Donly KJ, Ruiz M. In vitro demineralization inhibition of enamel caries utilizing an unfilled resin. Clin Prev Dent. 1992;14(6):22-24.
20. Silverstone LM. Structure of carious enamel, including the early lesion. Oral Sci Rev. 1973;3:100-160.
21. Meyer-Lueckel H, Paris S, Kielbassa AM. Surface layer erosion of natural caries lesions with phosphoric and hydrochloric acid gels in preparation for resin infiltration. Caries Res. 2007;41(3):223-230.
22. Paris S, Meyer-Lueckel H, Colfen H, et al. Penetration coefficients of commercially available and experimental composites intended to infiltrate enamel carious lesions. Dent Mater. 2007;23(6):742-748.
23. Paris S, Meyer-Lueckel H, Cölfen H, Kielbassa AM. Resin infiltration of artificial enamel caries lesions with experimental light curing resins. Dent Mater J. 2007;26(4):582-588.
24. Meyer-Lueckel H, Paris S. Progression of artificial enamel caries lesions after infiltration with experimental light curing resins. Caries Res. 2008;42(2):117-124.
25. Paris S, Bitter K, Renz H, et al. Validation of two dual fluorescence techniques for confocal microscopic visualization of resin penetration into enamel caries lesions. Microsc Res Tech. 2009;72(7):489-494.
27. Dalzell DP, Howes RI, Hubler PM. Microabrasion: effect of time, number of applications, and pressure on enamel loss. Pediatr Dent. 1995;17(3):207-211.
28. Tong LS, Pang MK, Mok NY, King NM, Wei SH. The effects of etching, micro-abrasion, and bleaching on surface enamel. J Dent Res. 1993;72(1): 67-71.
29. Croll TP. Hastening the enamel microabrasion procedure eliminating defects, cutting treatment time. J Am Dent Assoc. 1993;124(4):87-90.
30. Croll TP, Killian CM, Miller AS. Effect of enamel microabrasion compound on human gingiva: report of a case. Quintessence Int. 1990;21(12):959-963.
31. Fejerskov O. Changing paradigms in concepts on dental caries: consequences for oral health care. Caries Res. 2004;38(3): 182-191.